How Surgeons Kept a Man Alive With No Lungs for 48 Hours — And What It Means for Future Transplants
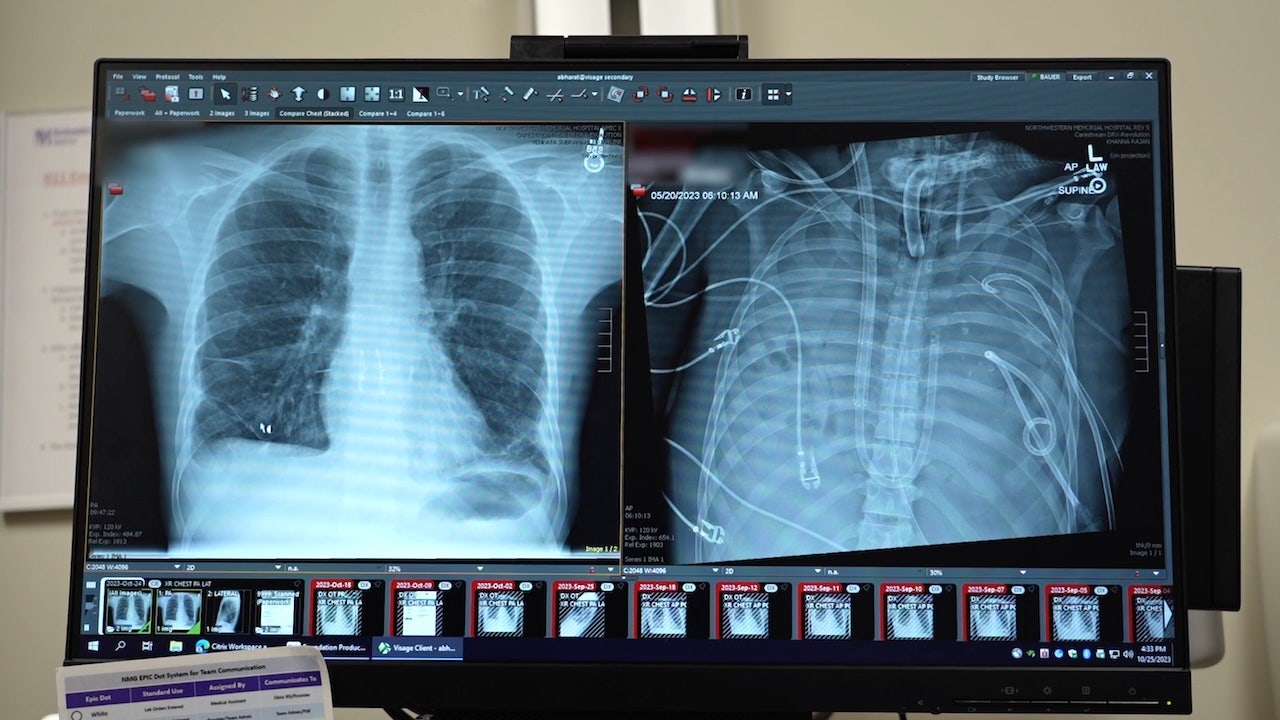
Surgeons at Northwestern Medicine in Chicago recently did something that sounds impossible at first glance: They kept a 33-year-old man alive for nearly 48 hours with no lungs inside his body while preparing him for a double-lung transplant. This innovative “bridge therapy” offers new hope for patients with severe lung infections and end-stage lung disease who might otherwise have no options left.
In this article, we’ll unpack what actually happened, how doctors managed to keep the patient alive without lungs, what this means for the future of lung transplants, and what patients and families facing similar situations can realistically expect.
If you or someone you love is living with advanced lung disease, stories like this can be both inspiring and overwhelming. Let’s walk through what this breakthrough really means—without the hype, but with genuine hope.
The Life-Threatening Problem: When Lungs Are Too Damaged to Wait
The patient in this case was battling a severe lung infection that left his lungs so badly damaged and infected that they were:
- Unable to provide enough oxygen to his body
- Actively spreading infection and inflammation
- Too risky to leave in place while waiting for donor lungs
Traditionally, even very sick patients must keep their diseased lungs until donor organs become available. But in this case, those lungs had become a deadly liability. The medical team faced a cruel paradox:
“We realized that leaving his infected lungs in place was killing him—but taking them out meant he would have no lungs at all. We had to create a bridge that didn’t exist yet.”
— Thoracic surgeon at Northwestern Medicine (case summary)
To break out of this dilemma, the team used a combination of advanced life-support technology and surgical innovation to keep the patient alive lung-free for nearly two days.
How Can Someone Live Without Lungs for 48 Hours?
The short answer is: by replacing the lungs’ gas-exchange function with sophisticated machines. The main technology involved is called ECMO (extracorporeal membrane oxygenation).
What ECMO Does
ECMO is often described as a “heart-lung machine,” but in this case it was used specifically to take over the role of the lungs:
- Blood is drawn out of the body through large tubes (cannulas).
- The blood passes through an artificial lung (membrane oxygenator) that adds oxygen and removes carbon dioxide.
- The oxygen-rich blood is then pumped back into the patient’s body.
Usually, ECMO supports damaged lungs while they heal. In this case, the lungs were removed entirely, and ECMO became the only way to oxygenate blood.

The Surgical “Bridge” Strategy
The Northwestern team used a multi-step plan often referred to as bridge therapy:
- Remove the infected lungs to stop the spread of infection and prevent further damage.
- Connect the patient to ECMO to fully replace lung function.
- Stabilize and monitor the patient for about 48 hours while awaiting suitable donor lungs.
- Perform a double-lung transplant once a compatible organ match was available.
Throughout this period, doctors had to carefully manage blood pressure, clotting, infection risk, and organ function. Even with today’s technology, surviving without lungs in place is extremely rare and high-risk.
Inside the Case: A 33-Year-Old’s Fight for Breath
According to the hospital’s report, the patient was a 33-year-old man in Missouri who developed a devastating lung infection. Despite intensive support, antibiotics, and ventilator care, his lungs continued to deteriorate.
He was transferred to Northwestern Medicine, one of the leading lung transplant centers in the United States, for evaluation. By the time he arrived, his:
- Oxygen levels were dangerously low
- Infection was overwhelming his lungs
- Overall condition was rapidly worsening, putting him at risk of multi-organ failure
The transplant team determined that:
- He was a good candidate for a double-lung transplant, but
- He would likely not survive long enough on his diseased lungs to receive donor organs
“We had to think differently. Removing the lungs before transplant is almost never done, but in his case, keeping them in was more dangerous than taking them out.”
— Transplant surgeon, Northwestern Medicine (paraphrased case commentary)
After a detailed discussion with the patient’s family about the extreme risks and uncertain outcomes, they agreed to proceed. His infected lungs were removed, he was placed on ECMO support, and two days later, he received a successful double-lung transplant.
Post-surgery, reports indicate that the patient’s new lungs functioned well, and he began the long but hopeful journey of rehabilitation and recovery.
The Science Behind This Breakthrough: Why It Matters
This case sits at the intersection of transplant medicine, critical care, and surgical innovation. It’s not the first time ECMO has been used as a bridge to lung transplant—but living with no lungs present for 48 hours is exceptionally rare.
What Makes This Different?
- Complete lung removal: Instead of supporting failing lungs, the team eliminated a major infection source by taking them out.
- Extended lung-free period: Nearly two days is a long time to rely entirely on artificial oxygenation.
- Potential new pathway: It demonstrates a new model for patients whose lungs are dangerously infected yet are still transplant candidates.
Earlier research in peer-reviewed journals has shown that ECMO can improve outcomes for select patients awaiting lung transplant, especially in cases of severe respiratory failure. This new case extends that concept further.

What Experts Are Saying
“Cases like this push the boundaries of what we thought was possible in transplant medicine. The key now is to study which patients can safely benefit from such extreme bridging strategies.”
— Academic transplant specialist commenting on novel bridge-to-transplant techniques
Who Could This Help in the Future?
This approach isn’t appropriate for everyone with lung disease. However, it may eventually offer a lifeline to specific high-risk groups, such as:
- Patients with severe, drug-resistant lung infections that make transplantation risky while infected lungs remain in place
- People with end-stage lung disease who are rapidly deteriorating while waiting for donor lungs
- Carefully selected patients in specialized transplant centers with access to ECMO and experienced surgical teams
It’s important to remember that every lung transplant case is unique. Many patients can successfully wait for donor lungs with standard support, without needing extreme measures like lung removal and ECMO-only bridge therapy.
Practical Guidance for Patients and Families Facing Lung Transplant Decisions
Hearing about dramatic success stories can stir up a lot of emotions—hope, fear, and sometimes frustration about what might or might not be possible in your situation. While this case is extraordinary, there are practical, grounded steps you can take today.
1. Ask About Your Center’s Experience and Options
- How many lung transplants does this hospital perform each year?
- Do they use ECMO as a bridge to transplant in selected cases?
- Are there partnerships with larger transplant centers if your case becomes highly complex?
2. Get a Second Opinion at a High-Volume Transplant Center
For complex or rapidly worsening lung disease, a second opinion from a major transplant center can:
- Confirm or clarify your eligibility for transplant
- Offer access to advanced therapies, including ECMO or clinical trials
- Provide realistic expectations about risks and potential outcomes
3. Prepare Questions for Difficult Conversations
Consider asking your care team:
- “What is the best-case, worst-case, and most likely scenario for me?”
- “If my condition worsens suddenly, what are the emergency options?”
- “Are there any advanced therapies (like ECMO) that might help in a crisis?”

Risks, Limits, and Ethical Considerations
As hopeful as this story is, it’s important to be clear about the very real risks involved in such extreme interventions.
Medical Risks
- Bleeding and clotting issues from ECMO and major surgery
- Infection risk from prolonged intensive care support
- Organ damage (kidneys, brain, heart) due to critical illness
- Graft rejection or complications after transplant
Ethical and Emotional Considerations
- Balancing the chance of survival against the risk of suffering
- Ensuring informed consent when emotions are running high
- Allocating scarce ICU and ECMO resources fairly
“Just because we can do something medically extraordinary doesn’t automatically mean we should. Each case requires careful, compassionate judgment.”
— Bioethicist specializing in critical care decisions
Key Takeaways for the Future of Lung Transplant Care
As we look ahead, this lung-free bridge case suggests several important possibilities:
- New strategies for patients with critically infected or destroyed lungs
- Growing role of ECMO in bridging selected patients to transplant
- Need for specialized centers capable of safely delivering such complex care
- Ongoing research to define who can benefit most—and who might be harmed—by extreme bridge therapies

For now, this case stands as a proof of concept—a dramatic example of what can happen when experienced surgeons, critical care teams, and transplant specialists work together at the very edge of what’s medically possible.
Moving Forward: How to Advocate for Yourself or a Loved One
If you’re living with severe lung disease or supporting someone who is, you don’t need a headline-making procedure to make a meaningful difference. You can start with grounded, practical steps:
- Talk openly with your pulmonologist about long-term planning, including if and when transplant evaluation makes sense.
- Request a referral to a regional or national transplant center if your disease is progressing.
- Bring a notebook (or use your phone) to record answers during appointments—you’re processing a lot.
- Lean on support groups (online or in person) for others living with lung disease or transplant experiences.
Medicine will keep evolving. New techniques—like keeping a patient alive without lungs for 48 hours—will continue to challenge what we think is possible. Amid all this change, what matters most is that you feel informed, heard, and supported in every decision.
Your next step: if this story resonates with your situation, schedule time with your care team this week to ask, “What are all of my options right now, and what might be possible if my condition worsens?”
