The Tiny Immune Switch That Could Transform Future Cancer Treatment
A Tiny Immune Switch With Big Potential: Blocking One Protein to Slow Cancer Growth
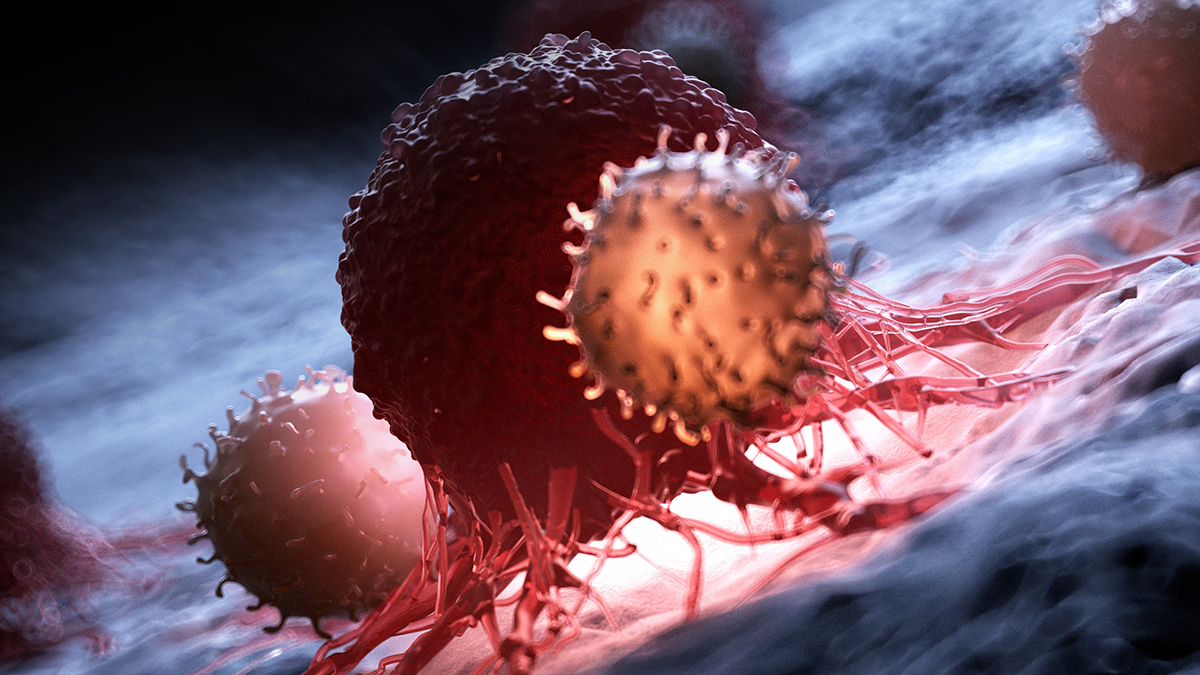
Researchers have discovered that blocking a single protein in mice can act like a molecular switch that boosts the immune system and slows cancer growth, opening the door to more precise, less toxic cancer treatments in the future. This article explains what the study found, how this immune switch works, what it might mean for human cancer therapies, and what patients and caregivers should realistically expect next.
If you or someone you love has faced cancer, you know how emotionally and physically exhausting treatment can be. Many people are now hearing about “immunotherapy” and wondering whether the next big breakthrough is just around the corner. A new mouse study reported by ScienceAlert suggests that targeting a single protein in immune cells may significantly slow tumor growth—but there are important nuances and caveats to understand.
Here, we’ll unpack the science in clear language, explore what this discovery could mean for future cancer therapies, and outline what is realistic to hope for right now.
The Challenge: Powerful Cancers and a Tired Immune System
Cancer is not just a “mass of bad cells.” It behaves more like a corrupt city, where tumor cells build defenses, hide from police (the immune system), and even recruit normal cells to help them grow. Modern cancer care increasingly focuses on making those “police”—your immune cells—more effective.
Immunotherapies like checkpoint inhibitors (for example, drugs targeting PD-1, PD-L1, or CTLA-4) have changed the outlook for some cancers. But:
- They work very well for a minority of patients.
- They can cause significant side effects when the immune system becomes overactive.
- Many tumors eventually learn to evade them.
Scientists are therefore searching for new “switches” inside immune cells that:
- Boost cancer-fighting activity, while
- Limiting collateral damage to healthy tissues.
“The immune system has many built-in brakes and accelerators. The art of immunotherapy is figuring out which ones we can safely adjust to improve anti-cancer responses.” — Adapted from educational materials by the U.S. National Cancer Institute.
The New Study: Blocking One Protein to Slow Cancer Growth in Mice
According to the ScienceAlert report, a research team has identified a specific protein in immune cells that acts like a molecular switch. In mouse models of cancer, blocking this protein:
- Reduced the speed of tumor growth.
- Enhanced the activity of certain immune cells that attack cancer.
- Appeared to “re-program” the tumor microenvironment to be less friendly to cancer.
While the finer details depend on the exact protein and pathways the researchers studied, the overall concept is this:
By turning off a key inhibitory protein, immune cells were better able to recognize, attack, and slow down the growth of cancer cells in mice.

How This Immune Switch Likely Works (in Plain Language)
Immune cells are constantly balancing two jobs:
- Protecting you from threats like cancer cells, viruses, and bacteria.
- Avoiding overreaction that could damage healthy tissue.
To manage this, they use a network of proteins that act as brakes and accelerators. This new research focuses on one of those brakes. When this protein is active:
- Immune cells become less aggressive.
- Tumors can grow with less resistance.
When the protein is blocked in mice:
- The brake is released.
- Immune cells recognize cancer cells more effectively.
- The tumor microenvironment becomes more hostile to cancer growth.

Before and After: What Changed in the Mice?
While every study differs, the general pattern described in this research looks something like this:
Before Blocking the Protein
- Tumors grew at their typical rate.
- Immune cells showed signs of “exhaustion” or reduced activity.
- The tumor environment supported cancer cell survival.
After Blocking the Protein
- Tumor growth slowed significantly in many of the mice.
- Immune cells were more active against cancer cells.
- The tumor microenvironment became less supportive of cancer growth.

It’s important to emphasize that this is slowing tumor growth, not necessarily eliminating tumors entirely. In mice, that can still be a powerful and clinically meaningful effect—especially if combined with other treatments.
What Could This Mean for Future Human Cancer Treatments?
Discoveries like this shape how researchers design the next generation of therapies. In the long term, blocking this protein might be used to:
- Enhance existing immunotherapies by giving immune cells an extra boost.
- Design more targeted drugs that activate only specific types of immune cells.
- Reduce reliance on high-dose chemotherapy in some settings, if immune-based approaches become more effective.
However, moving from mouse results to human treatments is a multi-step process that typically takes years:
- Confirm the protein’s role in human immune cells and cancer tissues.
- Develop safe, stable drugs (or biologics) that can precisely target this protein.
- Run early-phase clinical trials to evaluate safety in small groups of patients.
- Test effectiveness in larger, controlled clinical trials.
“Mouse studies are where many breakthroughs start, but careful, phased clinical trials are how we ensure those discoveries truly help people living with cancer.” — Medical oncologist, tertiary cancer center.
Important Limitations and Obstacles to Keep in Mind
Evidence-based medicine means getting excited about new ideas and being honest about their challenges. For this type of immune switch, key obstacles include:
- Mouse vs. human differences: An intervention that works in mice may not have the same effect in people.
- Immune-related side effects: Releasing a “brake” can trigger inflammation or autoimmunity if not carefully controlled.
- Tumor diversity: Different cancers may rely on different escape strategies; some may not respond to this particular protein block.
- Drug development hurdles: Creating a safe, effective drug that reaches the right cells at the right time is complex.
In other words, this discovery is encouraging, but it does not guarantee a new widely available treatment any time soon.

Practical Steps for Patients and Caregivers Right Now
While this specific protein-blocking approach is not yet a standard treatment, there are concrete things you can do today to stay connected to the latest, safest advances in cancer immunotherapy.
1. Talk with your oncology team about immunotherapy
- Ask whether approved immunotherapies are appropriate for your cancer type and stage.
- Discuss potential benefits, side effects, and alternatives.
- Inquire how your tumor’s specific biomarkers influence eligibility.
2. Explore clinical trial options from reliable sources
Clinical trials are where new strategies, like targeting molecular switches, are first tested in people. To find reputable trials:
- Use national databases such as ClinicalTrials.gov.
- Check major cancer centers and university hospitals in your region.
- Ask your oncologist to help interpret eligibility and risks.
3. Support your overall health during treatment
While lifestyle choices cannot replace cancer treatment, they can help you tolerate therapy better and support recovery:
- Focus on balanced nutrition as advised by a registered dietitian or oncology team.
- Engage in gentle physical activity when possible, like short walks, after medical clearance.
- Prioritize sleep and stress management (for example, mindfulness, counseling, or support groups).
How This Fits Into the Bigger Picture of Cancer Immunotherapy Research
Targeting single proteins in immune cells is part of a much larger research landscape. Over the past decade, scientists have:
- Developed checkpoint inhibitors that block proteins like PD-1/PD-L1 and CTLA-4, leading to major advances in some cancers.
- Created CAR T-cell therapies that re-engineer a patient’s own immune cells to attack specific targets.
- Investigated tumor vaccines and personalized neoantigen approaches.
The newly identified protein adds another potential target to this toolbox. If future research confirms its value in humans, it might be:
- Combined with checkpoint inhibitors to deepen responses.
- Incorporated into next-generation CAR T-cell designs.
- Used alongside radiation or chemotherapy to make tumors more visible to immune cells.
Authoritative organizations like the National Cancer Institute and Cancer Research UK provide regularly updated overviews of immunotherapy progress.
Staying Hopeful and Grounded as Cancer Research Moves Forward
The discovery that blocking a single protein can slow cancer growth in mice is a meaningful scientific step. It suggests that a carefully chosen immune switch can make tumors more vulnerable and the immune system more effective. At the same time, it remains an early-stage insight, not a treatment you can request from your doctor tomorrow.
Navigating cancer means living with uncertainty. You deserve information that is both hopeful and honest. As research progresses, your best tools are:
- A trusted relationship with your oncology team.
- Access to reliable, evidence-based resources.
- Support from family, friends, and patient communities.
If this kind of research interests you, consider:
- Asking your doctor how to stay informed about emerging immunotherapies.
- Exploring reputable clinical trials that match your situation.
- Sharing vetted resources with others in your support network.
Progress in cancer care often comes in many small steps that, over time, add up to life-changing advances. This new immune switch discovery is one such step—and many researchers around the world are working every day to turn findings like this into safer, more effective treatment options.
