Beyond Opioids: How Next‑Gen Gene Therapy May Tame Chronic Pain Without Addiction
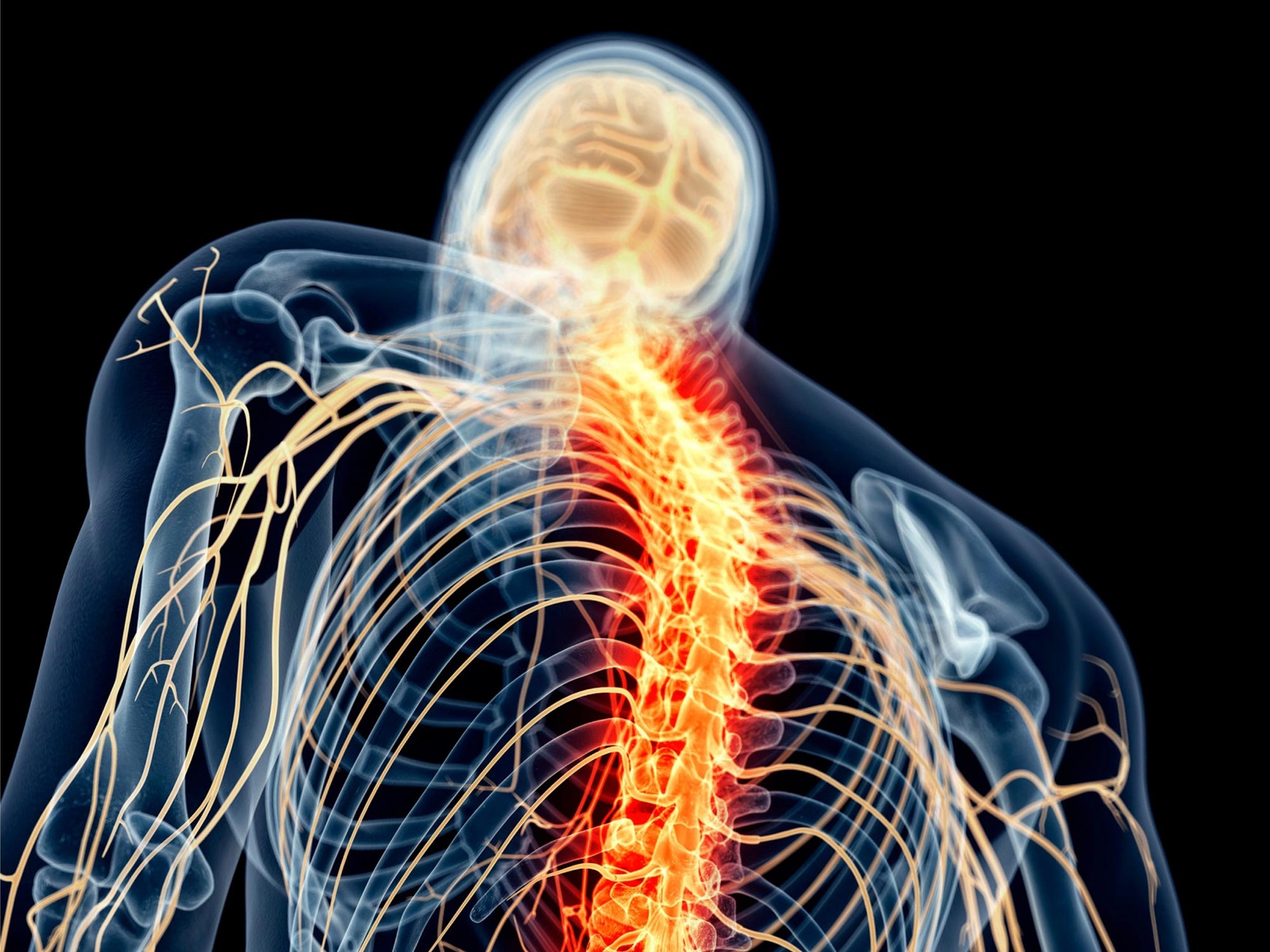
Chronic pain treatments often rely on opioids, which can bring serious risks of addiction and side effects. A new experimental gene therapy aims to calm pain-processing circuits in the brain and spinal cord without triggering the reward pathways that drive dependence, offering a glimpse of a future where long-term pain relief may not have to come at such a high cost.
If you live with chronic pain—or love someone who does—you know it affects far more than just the body. It shapes mood, sleep, relationships, and the simple ability to get through a day. Opioid medications have long been a mainstay for severe pain, but their potential for dependence and overdose has pushed researchers to look for safer, more precise options.
A recent preclinical study reported in SciTechDaily highlights a gene therapy that selectively targets pain-processing circuits in the brain. While it is not yet available for patients and still requires extensive testing, it offers an important proof of concept: it may be possible to shut down chronic pain at its source without lighting up the brain’s addiction pathways.
Why We Need Better Options Than Opioids for Chronic Pain
To appreciate why this new gene therapy matters, it helps to understand the bind many patients and clinicians are in today.
Opioids—such as oxycodone, hydrocodone, or morphine—can be effective for short-term, severe pain (like post-surgical pain or acute injury). But long-term use for chronic pain is much more complicated.
- Tolerance: Over time, the body adapts, and the same dose may no longer provide relief.
- Dependence and addiction risk: The brain’s reward systems are activated, and stopping suddenly can cause withdrawal.
- Side effects: Constipation, hormonal changes, sleep disruption, impaired breathing, and increased fall risk—especially in older adults.
- Overdose risk: Particularly when combined with alcohol, benzodiazepines, or other sedating medications.
“For most types of chronic pain, nonopioid therapies are preferred because they are at least as effective and carry less risk.”
— U.S. Centers for Disease Control and Prevention (CDC) Clinical Practice Guideline
Even with careful prescribing, some people find themselves stuck: non-opioid options don’t fully control their pain, yet opioids carry risks they don’t want to accept. That is the gap researchers are trying to fill with highly targeted treatments like this new gene therapy.
How the New Pain-Focused Gene Therapy Works
The study highlighted by SciTechDaily describes a gene therapy designed to act like a dimmer switch for chronic pain circuits while sparing the brain regions tied to reward and addiction.
Targeting Pain Circuits, Not the Whole Brain
Instead of flooding the body with a drug that affects many systems, this approach delivers genetic instructions directly to the nerve cells involved in processing pain signals. According to the report:
- The therapy uses an adeno-associated virus (AAV) vector, a commonly used delivery tool in gene therapy research.
- It is engineered to home in on pain-processing regions in the brain and, in some models, the spinal cord.
- Once inside target neurons, it drives the production of proteins that reduce the cells’ ability to transmit pain signals.
Why This Might Reduce Addiction Risk
Traditional opioids work broadly on mu-opioid receptors throughout the nervous system, including areas like the ventral tegmental area (VTA) and nucleus accumbens—key hubs in the brain’s reward circuitry. This broad action is part of what makes opioids both powerful pain relievers and potentially addictive.
In contrast, the new gene therapy is designed to:
- Localize its effects to pain-related pathways, such as specific spinal cord dorsal horn neurons or pain-processing brain regions.
- Avoid directly stimulating reward-related structures that drive craving and compulsive use.
- Provide durable changes in neural activity without daily dosing, which may reduce “chasing” effects some people experience with short-acting medications.
In preclinical animal models, the therapy:
- Reduced responses to chronic pain stimuli.
- Did not produce typical addiction-like behaviors seen with opioids (such as drug-seeking actions).
- Preserved normal functions like movement and general alertness, suggesting it was selectively modulating pain rather than sedating the animals.
“By focusing on discrete pain-processing circuits, we can, in principle, separate analgesia from reward. That’s the holy grail of non-addictive pain relief.”
— Neuroscientist involved in preclinical pain gene therapy research (paraphrased from current literature)
Gene Therapy vs. Opioids: A Side‑by‑Side Look
It’s too early to claim gene therapy will replace opioids. But comparing their potential strengths and limitations can help clarify what’s at stake.

Before & After: Conceptual View
Today (Opioid-centered approach):
- Broad action across the brain and body.
- Repeated daily dosing, sometimes for years.
- Risk of dependence, tolerance, and withdrawal.
- Potential cognitive and mood side effects.
Potential Future (Pain‑circuit gene therapy):
- Highly targeted delivery to pain-processing circuits.
- Single or infrequent treatments with long-lasting effects (based on current gene therapy models for other conditions).
- Designed to avoid reward pathways linked to addiction.
- Unknown long-term risks that must be thoroughly studied.
Where the Research Stands as of 2026
As of early 2026, the pain-targeted gene therapy described in SciTechDaily remains in the preclinical stage. That means:
- It has been tested in lab models (typically rodents) but not yet in human clinical trials.
- Researchers are still optimizing which genes to deliver, which brain or spinal regions to target, and what doses are safest.
- Regulatory agencies like the U.S. FDA will require extensive safety data before human trials are approved.
It’s also part of a broader movement in pain research. Other teams are exploring:
- Gene silencing for channels like Nav1.7, a sodium channel crucial for pain signaling.
- Optogenetic-like strategies adapted for potential clinical use, where light or designer drugs could toggle pain pathways on or off.
- Cell-based therapies that replace or reprogram pain-related neurons.
What makes the current study stand out is its focus on pain-processing regions of the brain and its explicit aim to decouple pain relief from reward pathways—addressing addiction risk head-on.
What This Means for You Right Now
It can be frustrating to hear about promising breakthroughs that aren’t yet available. Many people living with chronic pain wonder, “What am I supposed to do today?”
While we wait for more data on gene therapy, there are evidence-based steps you can take to improve pain control and reduce reliance on opioids where possible—always in partnership with your health-care team.
1. Talk With Your Clinician About a Multi‑Modal Pain Plan
Most guidelines now emphasize a multi-modal approach—combining several therapies, each targeting pain from a different angle:
- Non-opioid medications: NSAIDs, acetaminophen, certain antidepressants (e.g., SNRIs), and anti-seizure drugs (e.g., gabapentinoids) for nerve pain.
- Physical and occupational therapy: To rebuild strength, mobility, and functional independence.
- Psychological approaches: Cognitive behavioral therapy for pain, mindfulness-based stress reduction, and acceptance-and-commitment therapy.
- Interventional procedures: Nerve blocks, spinal injections, or implantable devices in select cases.
2. If You Use Opioids, Use Them Strategically
For some people, opioids remain part of a carefully monitored plan. Steps that can improve safety include:
- Reviewing your dose and duration regularly with your prescriber.
- Avoiding alcohol and other sedating drugs unless your clinician approves.
- Keeping naloxone (an overdose-reversal medication) on hand, especially at higher doses or when combined with other sedatives.
- Discussing gradual dose reductions if risks begin to outweigh benefits.
3. Stay Informed About Emerging Therapies
If you’re interested in future options like gene therapy:
- Let your pain specialist or neurologist know; they may be tracking clinical trial opportunities.
- Check reputable registries such as ClinicalTrials.gov using search terms like “chronic pain gene therapy.”
- Be cautious of clinics advertising “gene therapy” for pain outside of regulated trials—these often lack evidence and oversight.
Realistic Challenges and Ethical Questions Ahead
It’s important not to oversell what gene therapy can do for pain. Alongside its promise come serious questions that researchers, regulators, and patient communities will need to navigate carefully.
Safety and Long-Term Effects
- Irreversibility: Some gene therapies produce long-lasting changes that are difficult to “turn off” if problems arise.
- Immune reactions: The immune system can sometimes react strongly to viral vectors.
- Off-target effects: Genes might be delivered to unintended cells or regions, potentially altering functions beyond pain.
Access and Equity
Early gene therapies approved for other conditions have often been extremely expensive, raising concerns about who will have access if pain-focused treatments reach the clinic.
- Will insurers cover them?
- Will rural and underserved communities have access to specialized centers?
- How do we ensure that people with the greatest pain burdens aren’t left out?
Ethical Use
Because pain is subjective and deeply tied to quality of life, using powerful tools like gene therapy demands:
- Robust informed consent processes.
- Careful selection of candidates in early trials.
- Ongoing monitoring for unintended psychological or neurological changes.

Looking Ahead: A More Precise Future for Pain Care
The story of this new pain-focused gene therapy is, in many ways, the story of where pain medicine is headed: away from blunt instruments and toward precision.
For now, chronic pain is still managed with a mix of medications, physical approaches, and psychological support. Yet each incremental advance—from better non-opioid drugs to brain- and spinal cord–targeted therapies—moves us closer to treatments that:
- Calm the specific circuits driving your pain, not your entire nervous system.
- Offer relief without hijacking the reward pathways that fuel addiction.
- Respect your goals, values, and need for a life that feels like your own.

If you are living with chronic pain today, your next step isn’t to wait passively for gene therapy. It’s to work with a trusted clinician to build the best possible plan with the tools we already have—while keeping an eye on research that could expand your options in the years ahead.
Consider this your call-to-action: schedule a dedicated conversation with your health-care provider about your current pain plan, ask what non-opioid and multidisciplinary options might be added or optimized, and let them know you’re interested in emerging treatments so they can keep you in mind as the field evolves.
