This Simple Blood Test May Spot 50 Cancers Before Symptoms Start
New research suggests that multi-cancer early detection blood tests, which can screen for up to 50 cancers at once, are showing promising results in finding cancers earlier, when treatment is more effective. This article explains what these tests are, what the latest evidence shows, their benefits and limitations, and how they might fit into your future cancer screening plan.
If you’ve ever felt overwhelmed by the idea of cancer screening—different tests, different schedules, and the worry of missing something—you’re not alone. Scientists are now studying a new type of blood test that attempts to simplify things: one sample, potentially dozens of cancers detected, often before symptoms appear.
These “multi-cancer early detection” (MCED) tests are not yet a replacement for standard screening like mammograms or colonoscopies, but early data are encouraging. Let’s walk through what we know so far, what’s still uncertain, and how you can use this information to have a more informed conversation with your doctor.
What Are Multi-Cancer Early Detection Blood Tests?
Multi-cancer early detection (MCED) tests are blood tests designed to look for signals of many different cancers at the same time. Instead of checking for just one cancer—like a PSA test for prostate cancer—MCED tests analyze patterns in your blood that may indicate a tumor somewhere in the body.
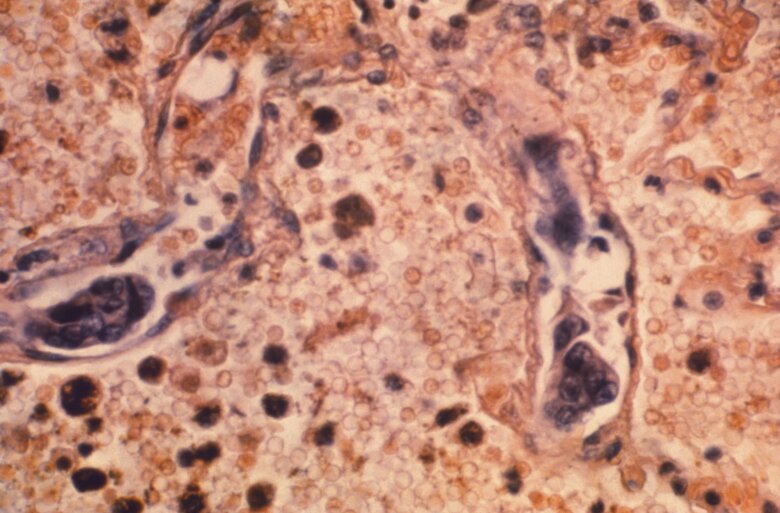
Most of these tests look for tiny fragments of tumor DNA (sometimes called circulating tumor DNA or ctDNA) and chemical markers attached to that DNA, known as epigenetic changes. Sophisticated algorithms then estimate:
- Whether a cancer signal is likely present
- What tissue or organ the signal may be coming from (for example, lung, colon, or pancreas)
- Sometimes, how strong that signal is, which can loosely relate to cancer stage
The goal is straightforward but ambitious: find more cancers at stage I or II, when options like surgery, targeted therapies, or radiation are more likely to cure or significantly control the disease.

What Do the Latest Findings Show About 50-Cancer Blood Tests?
Recent study updates, including data highlighted in outlets like WTOP, suggest that these blood tests can detect signals from more than 50 types of cancer, many of which currently have no routine screening (such as pancreatic, ovarian, and some rare cancers).
In large research programs, including trials in the U.S. and U.K., early results show:
- Feasibility: It’s technically possible to screen for dozens of cancers from a single blood draw.
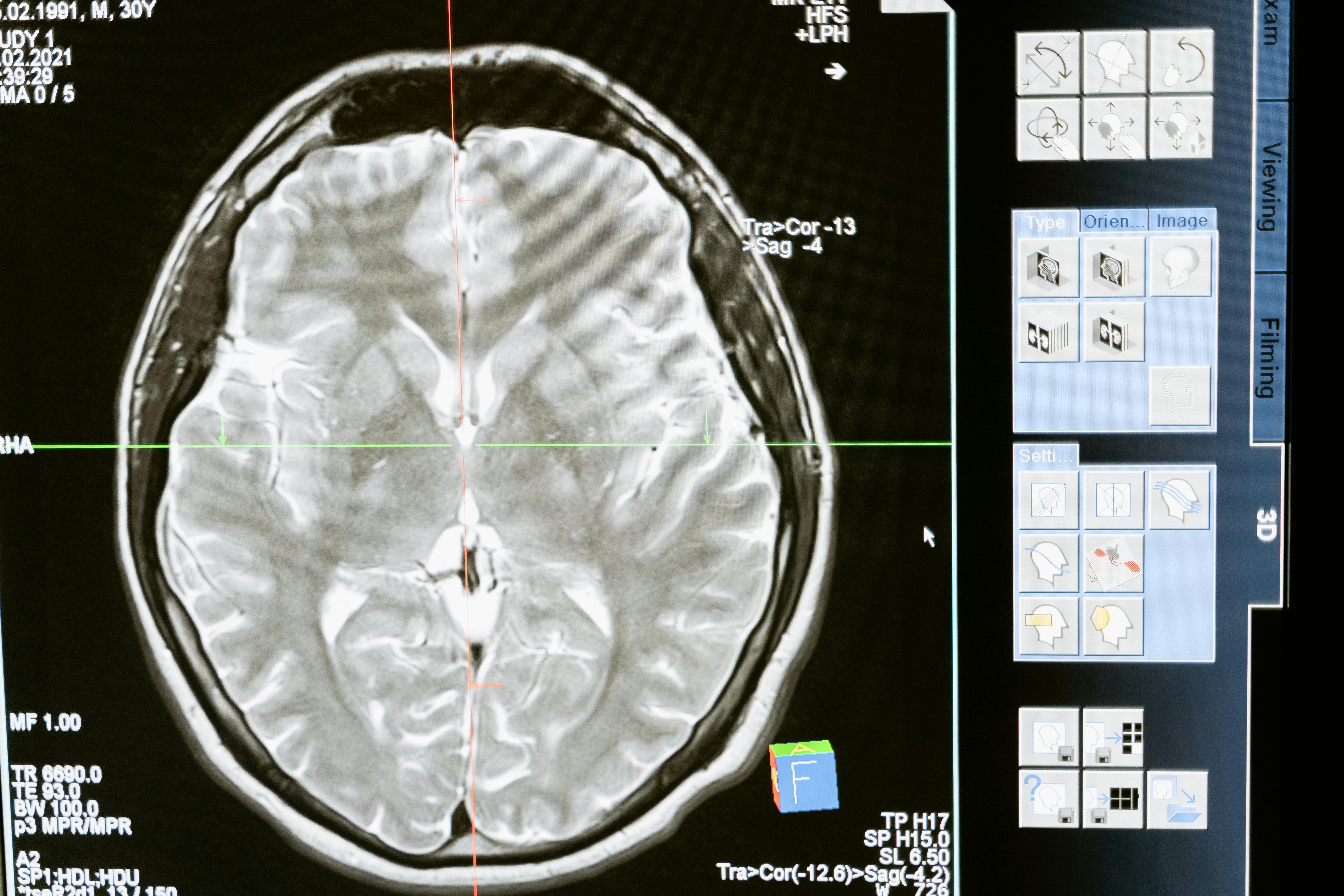
- Stage shift: A higher proportion of cancers are being found at earlier stages in participants offered MCED testing, compared to typical diagnosis patterns in the community.
- Tissue-of-origin accuracy: When a cancer signal is detected, the tests can often suggest the likely organ system, helping doctors decide what imaging or follow-up tests to order.
“These multi-cancer blood tests are among the most promising tools we’ve seen for shifting cancer diagnosis to earlier stages. But we’re still in the validation phase—we need to be sure they save lives overall, not just find more cancers.”
— Oncologist involved in early-detection research
Importantly, the studies so far focus on how well the tests detect cancer and how often they give false alarms. The next crucial step is proving that using these tests routinely actually reduces deaths from cancer and does so without causing too much unnecessary testing or anxiety.
How These 50-Cancer Blood Tests Work in Practice
While each company’s test is a bit different, the process for patients is surprisingly simple:
- Blood draw: A standard blood sample is taken in a clinic or lab.
- Lab analysis: The sample is analyzed for patterns in DNA and other markers associated with many cancers.
- Result report: The result generally comes back as either “no cancer signal detected” or “cancer signal detected,” sometimes with a suggested tissue of origin.
- Follow-up testing: If a signal is detected, your clinician typically orders imaging (such as CT, MRI, or ultrasound) and sometimes targeted diagnostic tests to confirm or rule out cancer.
From the patient’s standpoint, it can feel almost too easy compared with traditional screenings. But the simple blood draw hides a very complex reality: a positive test is only the beginning of an often detailed—and occasionally stressful—diagnostic journey.
Potential Benefits: Why These Tests Are Generating Excitement
The enthusiasm around multi-cancer early detection blood tests stems from several potential advantages over our current patchwork of screenings.
- Earlier diagnosis for hard-to-detect cancers
Many of the deadliest cancers—like pancreatic, ovarian, and liver cancer—are often discovered late. MCED tests aim to catch some of these before symptoms arise. - Convenience and simplicity
One blood draw could screen for dozens of cancers at once, which may improve screening participation over time. - Broader coverage
Right now, routine screening only exists for a handful of cancers. An MCED test could, in theory, expand coverage to many more. - Complement to existing tests
Researchers see MCED as an addition—not a substitute—to proven tests like colonoscopies and mammograms, potentially catching cancers between standard screenings.
Important Limitations and Risks You Should Know
Despite the promising data, these tests come with real limitations. Understanding them is essential before considering any new screening option.
- They can miss cancers (false negatives)
Not every cancer sheds detectable DNA into the bloodstream, especially the smallest and earliest ones. A “no signal detected” result does not guarantee that you are cancer-free. - They can raise false alarms (false positives)
Some people will receive a “cancer signal detected” result, go through extensive testing, and ultimately be told no cancer was found. That process can be stressful, time-consuming, and sometimes risky. - Overdiagnosis
These tests may detect slow-growing cancers that might never have caused symptoms or shortened life. Treating all of them aggressively can lead to side effects without clear benefit. - Cost and access
Today, most MCED tests are not covered by insurance and can be expensive. That raises concerns about equity and who gets access if they prove beneficial. - Unclear best use
We don’t yet know who benefits most—average-risk adults, older adults, or those at higher genetic or family risk. Guidelines are still being developed.
“We need to be honest: no test is perfect, and more testing can sometimes cause harm. Our responsibility is to find the balance where benefits clearly outweigh the risks.”
— Public health researcher specializing in cancer screening
MCED Blood Tests vs. Traditional Cancer Screening
It’s helpful to think of MCED tests as a possible extra layer of screening, not as a replacement for what already works.
Today’s proven screening tools:
- Mammography (breast cancer)
- Colonoscopy or stool-based tests (colorectal cancer)
- Pap test and HPV test (cervical cancer)
- Low-dose CT scans for some people at high risk of lung cancer (such as long-term heavy smokers)
These tests have something MCEDs don’t yet have: clear evidence that they reduce deaths in specific age and risk groups.
In the future, guidelines may suggest:
- Continuing standard screenings on schedule
- Adding an MCED blood test at certain ages or risk levels
- Using MCED results to tailor follow-up imaging or diagnostic tests
Who Might Consider a Multi-Cancer Blood Test Right Now?
Because these tests are still being evaluated, they are generally not part of routine care for most people. Today, they may be considered in a few scenarios:
- Within a clinical trial
This is often the best way to access MCED tests. You receive close monitoring, and your experience contributes to research that shapes future guidelines. - Through a specialist consultation
Some oncology or high-risk clinics may offer MCED tests selectively, typically after a careful discussion of pros and cons. - Self-pay testing
Some commercial tests may be offered directly to patients via clinicians, but usually at significant out-of-pocket cost and with variable insurance coverage.
If you are curious, especially if you have a strong family history of cancer or known genetic risk factors (like BRCA1/2), start with your primary care clinician or genetic counselor. They can help you weigh:
- Your current proven screening needs (which should come first)
- Whether a trial or MCED test is available and appropriate
- Your personal feelings about uncertainty, possible false positives, and cost
How to Talk with Your Doctor About 50-Cancer Blood Tests
Bringing up a new technology with your doctor can feel intimidating. A structured conversation can make it easier.
Consider asking:
- “Am I up to date on all recommended cancer screenings for my age and risk?”
- “Given my family history, do I qualify for any additional screening or genetic testing?”
- “What do you think about multi-cancer early detection blood tests for someone like me?”
- “Are there any clinical trials nearby that involve these tests?”
- “If an MCED test were positive, what would the next steps look like?”
Common Concerns and How to Navigate Them
Even if the science is compelling, real-world worries are completely valid. Here are a few of the most common, along with practical ways to address them.
- “I’m afraid of getting a false alarm.”
Ask your doctor about the positive predictive value of the test—how often a positive result really means cancer in your age group. Discuss in advance what follow-up testing would look like and how to support your mental health during any waiting period. - “I don’t want to be over-tested.”
Clarify how often the test would be repeated (if at all), and whether it would lead to routine extra scans or procedures even if you feel well. - “I’m worried about cost.”
Before considering any MCED test outside of a trial, ask for a clear estimate of your out-of-pocket expenses and whether financial assistance or research options exist. - “I’m overwhelmed by all the information.”
It’s okay to take your time. You can always decide to focus first on proven screenings and revisit MCED testing later as evidence and guidelines become clearer.

What Research Still Needs to Show
The next few years are critical. Large, long-term studies are underway to answer key questions:
- Do MCED tests reduce deaths from cancer when used in real-world populations?
- What is the best age or risk profile to start testing?
- How often should testing be done to balance benefit and harm?
- What are the psychological impacts on patients and families?
- How can access be made equitable across different communities?
Until we have clear answers, most medical societies recommend treating MCED tests as experimental tools, ideally used in the context of research or careful shared decision-making with a knowledgeable clinician.
Bringing It All Together: A Practical Way Forward
Multi-cancer early detection blood tests—some capable of screening for up to 50 cancers at once—represent one of the most intriguing frontiers in cancer prevention. The early data are encouraging: more cancers found, and often at earlier stages.
At the same time, they are not magic bullets. They can miss cancers, raise false alarms, and are not yet proven to reduce deaths when used broadly. For now, they’re best viewed as promising tools under active study, not replacements for the screening tests we already know save lives.
A grounded, step-by-step approach might look like this:
- Make sure you’re current on established cancer screenings for your age and risk.
- Review your family history and discuss any hereditary risk with your clinician.
- Ask about relevant clinical trials or research programs in your area.
- Consider MCED testing only after understanding possible benefits, limits, costs, and follow-up plans.
You don’t have to navigate this alone.
Your next best step is simple and actionable: schedule a conversation with your primary care doctor or oncology team and bring this topic to the table. By combining emerging tools like multi-cancer blood tests with time-tested screenings and healthy lifestyle choices, you give yourself the best chance of catching problems early—without losing sight of your overall well-being.
