Sewage Is Whispering Warnings: What Wastewater Can Tell Us About the Next Antibiotic-Resistant Superbug
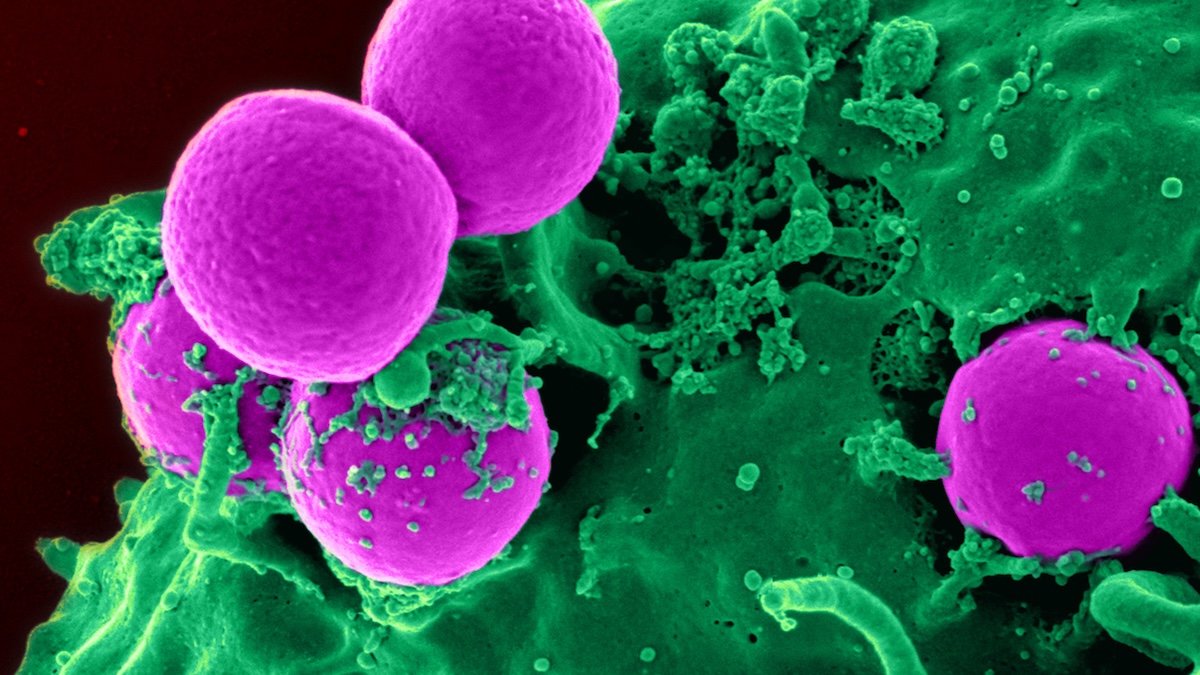
Antibiotic-resistant superbugs are quietly spreading around the world, and new research shows that our sewage systems are already carrying genetic warning signs of tomorrow’s drug‑defying infections. By listening closely to what flows through wastewater, scientists can spot emerging antimicrobial resistance earlier, giving health systems and communities a chance to respond before routine infections become life‑threatening again.
If you’ve ever had an infection that cleared up after a course of antibiotics, you’ve personally benefited from one of medicine’s greatest inventions. But that quiet confidence—“the doctor will give me something and it’ll go away”—is exactly what’s now at risk. Dangerous microbes are rapidly evolving ways to defy our best medications, a global crisis called antimicrobial resistance (AMR).
A recent analysis highlighted by ScienceAlert points to an unexpected early‑warning system: our sewage. From hospital drains to household toilets, wastewater is turning out to be a powerful lens into how resistance genes are spreading long before we see full‑blown hospital outbreaks.
What Is Antimicrobial Resistance—and Why Sewage Is Involved
Antimicrobial resistance happens when bacteria, viruses, fungi, or parasites adapt so that drugs—like antibiotics, antivirals, or antifungals—no longer work well against them. The World Health Organization estimates that millions of infections each year are already harder to treat because of AMR, and by mid‑century, resistant infections could kill more people annually than cancer if we don’t change course.
The ScienceAlert report covers new research showing that:
- Sewage samples from cities around the world contain a rich mix of resistance genes, including some that are rare or not yet common in nearby hospitals.
- These “grim signals” can reveal future resistance threats—genes that might spread into widely circulating superbugs.
- Wastewater monitoring can act as a surveillance radar for AMR, similar to how it was used during COVID‑19 to track virus levels.
How Sewage Becomes a Crystal Ball for Superbugs
It might sound unpleasant, but from a scientific point of view, sewage is incredibly informative. It pools together what’s happening across thousands—or even millions—of people.
- Sampling: Researchers collect wastewater from treatment plants, hospital drains, or even specific neighborhoods.
- Sequencing DNA: They use metagenomic sequencing to read all the genetic material in the sample, including bacterial DNA and resistance genes.
- Tracking resistance genes: By comparing these genes to known databases, scientists can see:
- Which antibiotics local microbes are learning to resist.
- Where new or rare resistance genes first appear.
- How patterns change over weeks, months, and years.
“Wastewater surveillance lets us see resistance threats emerging in real time, often before patients ever show up in hospital wards.”

The latest findings suggest that some resistance genes found in sewage are not yet common in clinical samples but have the potential to spread. In other words, sewage is revealing tomorrow’s problems today.
Why Future Antimicrobial Resistance Signals Are So Concerning
When researchers talk about “grim signals,” they’re not trying to be dramatic. They’re pointing out three uncomfortable truths about antimicrobial resistance:
- Resistant genes can spread faster than we detect them clinically.
By the time a hospital reports clusters of hard‑to‑treat infections, those genes may already be entrenched in the community. - Environmental hotspots matter.
Wastewater carries residues of antibiotics from hospitals, farms, and households. These low, chronic levels of drugs can encourage microbes to evolve resistance, even outside of direct medical use. - Routine infections could become risky again.
Simple urinary tract infections, skin infections, or post‑surgery complications become far more dangerous when first‑line antibiotics fail.
A Real-World Glimpse: When an Easy Infection Isn’t Easy Anymore
In one European city that began wastewater monitoring after COVID‑19, public health teams noticed a sudden rise in genes linked to resistance against a “last‑resort” antibiotic called carbapenem. At the time, local hospitals weren’t yet seeing a surge in resistant infections.
Over the next year, sporadic cases of carbapenem‑resistant infections began appearing in wards that treat vulnerable patients—those recovering from surgery or chemotherapy. Because wastewater had already raised a flag, hospitals there:
- Reviewed antibiotic prescribing practices.
- Stepped up screening of high‑risk patients.
- Improved cleaning and hand‑hygiene audits.
This isn’t a miracle story where resistance disappears overnight. But it shows how early signals from sewage gave clinicians a head start, likely preventing a larger outbreak.
What You Can Do About Antimicrobial Resistance (Yes, You)
AMR can feel overwhelming and abstract—especially when we’re talking about genes in sewage. But everyday choices genuinely influence how fast resistance spreads.
1. Use Antibiotics Wisely
- Only take antibiotics when prescribed by a licensed professional.
- Don’t pressure your doctor for antibiotics if they say a virus (like a cold or flu) is the cause.
- Finish the full course exactly as directed—stopping early can help the toughest bacteria survive.
- Never share leftovers or use someone else’s prescription.
2. Prevent Infections in the First Place
- Stay up to date with recommended vaccinations.
- Practice regular handwashing, especially before eating and after using the bathroom.
- Follow wound‑care instructions after surgery or injuries.
3. Be Mindful With Animals and Food
- Use antibiotics in pets only under veterinary guidance.
- Handle raw meat safely and cook thoroughly.
- Support policies or producers that aim to reduce routine antibiotic use in livestock where possible.

How Governments and Health Systems Can Use Sewage Surveillance
While individuals make a difference, the full power of sewage‑based AMR monitoring lies in public health and policy. The ScienceAlert‑covered research adds weight to several key strategies:
- Build routine wastewater monitoring networks.
Cities and regions can treat sewage sampling like weather forecasting for microbes—regular, standardized, and shared with decision‑makers. - Integrate data with hospitals and labs.
Linking wastewater results with clinical data helps detect when resistance moves from “genes in the environment” into real patient infections. - Guide antibiotic stewardship.
If sewage shows rising genes against specific drugs, hospitals can:- Review how often those drugs are prescribed.
- Update treatment guidelines.
- Strengthen infection‑prevention protocols.
- Improve wastewater treatment and sanitation.
Stronger treatment systems can reduce the load of resistant bacteria and genes entering rivers, soil, and eventually food chains.
What the Science Says: Evidence Behind the Warnings
Multiple lines of research now support the idea that wastewater is a powerful tool for tracking antimicrobial resistance:
- Global mapping projects have shown that resistance gene profiles in sewage mirror local antibiotic use and prescribing patterns.
- Studies comparing hospital and community wastewater find clinically relevant resistance genes—such as ESBLs and carbapenemases—long before large outbreaks appear.
- During COVID‑19, wastewater successfully tracked SARS‑CoV‑2 trends, proving that population‑level surveillance via sewage is feasible and cost‑effective.
For deeper reading, see:
- World Health Organization – Antimicrobial Resistance Overview
- Centers for Disease Control and Prevention – Antibiotic / Antimicrobial Resistance
- European Centre for Disease Prevention and Control – AMR Surveillance in Europe

Common Obstacles—and How We Can Overcome Them
Even with compelling data, expanding sewage‑based AMR surveillance faces real‑world barriers:
- Funding and infrastructure: Not all regions have the lab capacity or budget for routine sequencing.
Possible solutions: regional shared labs, international funding, and cheaper sequencing technologies. - Data interpretation: Sewage contains a mix of microbes from humans, animals, industry, and the environment.
Possible solutions: standardized methods and open databases to compare results across countries. - Political will: AMR doesn’t produce dramatic headlines like a sudden pandemic, so it’s easy to postpone action.
Possible solutions: clear communication about the economic costs of inaction, and integrating AMR metrics into national health planning.
Before and After: A World With and Without Strong AMR Surveillance
To put the stakes in perspective, imagine two futures:
- Future A – We invest in AMR surveillance, including sewage monitoring:
- Hospitals get early warnings about new resistance trends.
- Doctors adjust treatment guidelines proactively.
- Most routine surgeries and infections remain relatively safe.
- Future B – We ignore early warning signs:
- Resistant strains spread silently until standard antibiotics fail widely.
- More people need second‑ or third‑line drugs with higher costs and side‑effect risks.
- Procedures we now consider routine—like joint replacements or C‑sections—carry higher danger.
The ScienceAlert coverage of grim signals in sewage is essentially a nudge toward Future A. We still have time to choose.
Turning Grim Signals Into Early Warnings We Can Act On
It’s understandable to feel uneasy when you hear that sewage is filled with the genetic seeds of future superbugs. But unease can be useful if it leads to thoughtful action instead of panic.
The story behind those wastewater findings is not that we’re doomed—it’s that we’re finally learning to listen earlier. The same methods that uncovered “grim signals” of future antimicrobial resistance can also guide smarter policies, better prescribing, and more targeted infection control.
You don’t need to be a scientist or policymaker to contribute. By using antibiotics carefully, practicing everyday infection‑prevention habits, and supporting evidence‑based health policies, you’re part of a global effort to keep these medicines working.
Call to action: Next time you’re prescribed an antibiotic, ask one simple question—“Is this truly necessary, and how can I use it responsibly?” Small conversations like that, multiplied across millions of people, can change our trajectory on antimicrobial resistance.
