Should You Take Supplements to Prevent Cancer? An Oncologist Breaks Down the Science
Cancer and Supplements: Clearing Up the Confusion
If you or someone you love has faced cancer, you’ve probably wondered: “Should I be taking supplements to boost my immunity or fight the cancer?” It’s an understandable question. Shelves are lined with pills that promise antioxidant power, immune support, and “cell protection.” But the science is far more nuanced than most marketing slogans—and sometimes, the very supplements that feel “natural” and safe can actually increase risk or interfere with treatment.
As oncologists, especially those who treat people with leukemia and other bone-marrow cancers, we routinely review long lists of vitamins, herbal products, and powders our patients are taking. Most are harmless. A few can be helpful. And some, in certain situations, clearly warrant caution or even stopping altogether.

This guide walks through what current research (up to early 2026) says about cancer and supplements, and how to make informed, realistic decisions with your care team.
Why Supplements Are So Tempting During Cancer
Cancer shakes your sense of control. Swallowing a capsule that promises extra defense can feel like something concrete you can do right now. Family and friends often enthusiastically recommend products they’ve read about online or seen in ads, hoping to help.
The problem is that:
- Supplement quality and dosing are highly variable.
- “Natural” does not automatically mean safe—especially in immunocompromised people.
- Some high-dose vitamins and herbs can change how chemotherapy, immunotherapy, or hormonal therapies work.
- Marketing claims are not the same as evidence from rigorous clinical trials.
“In oncology clinic, we find that most supplements are neutral, a few are beneficial, but a small number are clearly harmful or risky when used in the wrong context.”
What the Science Says: Supplements and Cancer Risk
Research on supplements and cancer comes from several kinds of studies:
- Observational studies – watch what people already do and see who gets cancer.
- Randomized controlled trials (RCTs) – assign people to supplement vs. placebo and follow outcomes.
- Laboratory/animal studies – look at mechanisms in cells or mice.
Lab studies often show that certain compounds can slow cancer cells in a dish. But that doesn’t mean swallowing large doses in humans has the same effect—or is even safe.

Some of the most important findings from large RCTs include:
- Beta-carotene and lung cancer: In smokers and asbestos-exposed workers, high-dose beta-carotene supplements increased lung cancer risk rather than reducing it.
- Vitamin E and prostate cancer: The SELECT trial found that vitamin E supplements were associated with a higher risk of prostate cancer in generally healthy men.
- Folic acid: Necessary for health in normal amounts, but some studies suggest that excess supplemental folic acid might promote growth of existing precancerous lesions.
Overall, for most people, a balanced diet is more consistently linked to reduced cancer risk than any single vitamin pill.
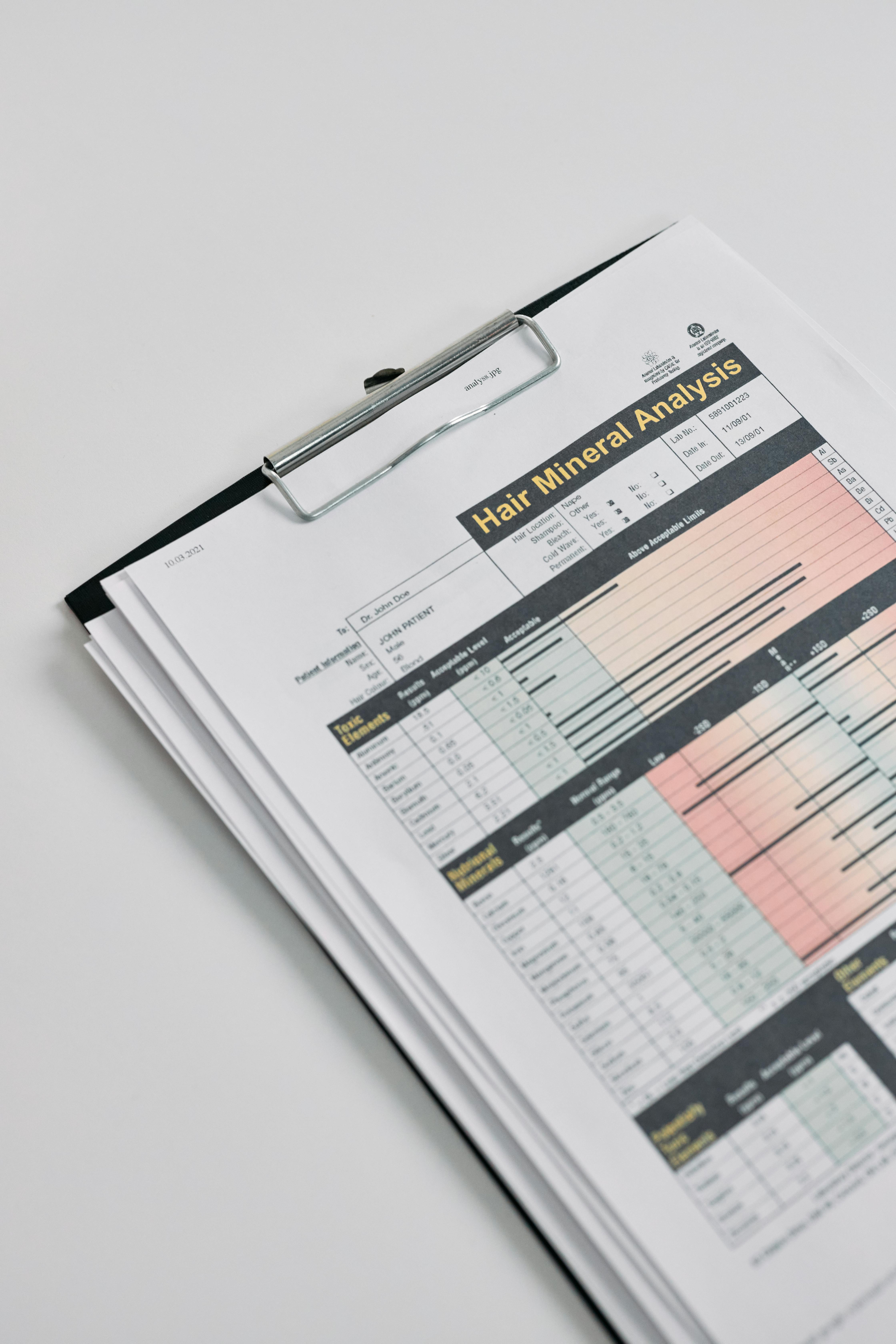
Common Supplements in Cancer Care: Helpful, Neutral, or Risky?
Below is a simplified overview of how several widely used supplements relate to cancer, based on studies available through early 2026. Effects can differ by dose, timing, and individual health status.
1. Multivitamins
Standard-dose multivitamins (around 100% of daily needs) are generally considered safe for most people and may be reasonable if your diet is limited— for example, during chemotherapy when appetite is poor.
- No strong evidence they prevent cancer in otherwise well-nourished adults.
- May help correct minor deficiencies, which can support overall health.
2. Vitamin D
Low vitamin D levels are common, and deficiency is linked with worse outcomes in several cancers, though it’s not always clear if deficiency causes worse outcomes or simply reflects poorer health.
- Moderate supplementation to correct true deficiency is widely accepted.
- Very high doses (well above typical prescribed amounts) are not proven to improve cancer survival and can cause harm, including elevated calcium and kidney issues.
Work with your doctor to check blood levels before assuming “more is better.”
3. Antioxidant Vitamins (C, E, A, high-dose mixtures)
Antioxidants are often marketed as “cancer fighters,” but timing and dose matter.
- High-dose antioxidants during radiation or certain chemotherapies may, in theory, protect cancer cells from the very oxidative damage those treatments are meant to cause.
- Randomized trials have not shown clear survival benefits from high doses during treatment.
- Normal dietary intake from fruits and vegetables remains strongly recommended.
4. Herbal Products (e.g., turmeric/curcumin, green tea extract, St. John’s wort)
Herbal products are particularly complex. Composition varies widely between brands, and they often affect liver enzymes that metabolize chemotherapy or hormonal drugs.
- St. John’s wort can significantly reduce blood levels of certain cancer drugs and is usually discouraged during treatment.
- Concentrated green tea extracts have been linked, in rare cases, to liver toxicity at high doses.
- Curcumin has interesting lab data, but clinical evidence is still limited; it can alter drug metabolism at higher doses.
5. Probiotics
The gut microbiome is increasingly recognized as important in cancer treatment response. However, for people with severely impaired immunity—such as those with leukemia or after bone marrow transplant—live bacteria in some probiotics can rarely cause bloodstream infections.
- In otherwise stable individuals, selected probiotics may support digestive health.
- In highly immunocompromised patients, many centers advise avoiding probiotics unless recommended by your team.
A Real-World Scenario: When “Just Vitamins” Aren’t So Simple
In clinic, I once reviewed the medication list of a man being treated for leukemia. Alongside his chemotherapy, he was taking a “natural immune support” blend from a health store—eight different herbs, high-dose antioxidants, and probiotics. He felt sure it was helping him tolerate treatment.
When we checked the specific ingredients, we found:
- Two herbs known to affect liver enzymes that process his chemotherapy.
- Vitamin E at a dose associated with increased bleeding risk.
- Live bacterial strains that our transplant service routinely avoids in severely immunocompromised patients.
Together, we decided to:
- Pause the blend during intensive chemotherapy.
- Replace it with a simple, standard-dose multivitamin.
- Focus on nutrition, movement as tolerated, and sleep as his main “immune support.”
He was relieved—not because we banned all supplements, but because he finally had a plan grounded in evidence and tailored to his situation.
How to Use Supplements Safely During and After Cancer
You don’t need to manage this alone. Here’s a practical step-by-step approach you can bring to your next appointment.
- Make a complete list.
Include every vitamin, mineral, powder, herbal product, and “immune booster.” Note the brand, dose, and how often you take it.
- Share the list with your oncologist and pharmacist.
Ask specifically: “Do any of these interact with my chemo, immunotherapy, or other medications?” and “Should I stop any during treatment?”
- Prioritize correcting real deficiencies.
If labs show low vitamin D, B12, iron, or others, targeted supplementation is usually more useful than broad mega-dosing.
- Avoid mega-doses unless prescribed.
More is not always better. Staying near recommended daily intakes is safer unless your clinician advises otherwise for a specific reason.
- Focus on diet first.
Work with a registered dietitian experienced in oncology to build an eating pattern that supports your treatment and recovery. Supplements should “supplement,” not replace, food.
Before vs. After: A Smarter Supplement Strategy
Many patients begin their cancer journey taking a patchwork of pills based on internet searches and well-meaning advice. With a little structure, that can shift to a safer, more effective plan.
| Before | After |
|---|---|
| Multiple high-dose single vitamins and herbs | Standard-dose multivitamin plus only needed targeted supplements |
| Unknown interactions with chemo and transplant meds | Pharmacist-reviewed list with high-risk products removed |
| Focus on pills as primary defense | Focus on nutrition, physical activity, sleep, and mental health |

Common Obstacles—and How to Navigate Them
Even when you understand the science, real-life barriers can make it hard to change your supplement routine.
- “I’m afraid to stop anything in case it’s helping.”
It’s natural to worry. Try framing changes as a trial you’re doing together with your team, based on what we know today. You can always re-evaluate.
- Pressure from friends or online communities.
Thank them for caring, then explain that your plan is guided by your oncology team and evidence from clinical trials—not by what works for someone else’s body and cancer.
- Fatigue and brain fog.
Ask a trusted person to help organize medication boxes, track doses, and update your supplement list for appointments.
“The goal isn’t to strip away hope—it’s to direct your effort and resources toward the strategies that give you the best chance, based on what we actually know.”
Where to Find Reliable, Up-to-Date Information
Claims about supplements evolve as new studies are published. To keep perspective:
- Check reputable cancer organizations for supplement information, such as:
- Look for information that:
- References specific clinical trials or systematic reviews.
- Admits uncertainty where it exists.
- Avoids promises of “cures” or instant results.
Putting It All Together: A Balanced, Evidence-Based Approach
Supplements can play a small, carefully chosen role in cancer care—especially to correct true deficiencies or support nutrition when eating is difficult. But they are not a substitute for proven therapies, and in certain situations, they can add real risk.
You deserve a plan that respects both your hope and the current state of the science.
- Use supplements to fill gaps, not as magic bullets.
- Avoid high doses and complex herbal blends unless specifically recommended.
- Make every capsule part of an open conversation with your oncology team.
At your next visit, bring your full supplement list and ask: “Given what we know today, which of these truly support my care, and which might be better to pause?” That simple question can help transform a confusing mix of pills into a thoughtful, evidence-guided strategy tailored to you.
