Scientists Are Rewriting Kidney Transplants With a Universal Donor Breakthrough
Scientists are developing a “universal” kidney that can match any blood type, a breakthrough that could shorten transplant waiting lists and save lives by making more donor organs compatible with more patients. If you or someone you love has ever waited for a transplant, you know how agonizing every day on that list can feel. This emerging research doesn’t magically fix the system overnight, but it does point to a future where blood type is no longer such a rigid barrier.
After more than a decade of work, researchers have shown it’s possible to take a donor kidney and strip away the blood-type markers that would normally cause rejection in a mismatched recipient. In this guide, we’ll unpack what this “universal kidney” actually means, how it works, what the early data show, and what patients and families can realistically expect over the coming years.
The Problem: Blood Type Still Blocks Too Many Kidney Transplants
Worldwide, kidney disease is one of the leading causes of serious illness and early death. For people with end-stage kidney disease, dialysis can keep them alive, but a transplant almost always offers a longer and better-quality life. The hard part is getting that transplant in time.
- Kidneys must be matched by blood type (A, B, AB, or O) and other immune markers.
- Patients with rarer blood types, especially type B and some ethnic minorities, can wait years longer.
- Many donor kidneys are never used for a specific patient because the blood types don’t line up.
“Right now, a perfectly healthy donor kidney might not be used for the person who needs it most—simply because of blood type. If we can safely remove that barrier, we can make the system much more efficient and more fair.”
— Transplant nephrologist quoted in recent clinical discussions
For families, these statistics are painfully personal. In transplant clinics, it’s common to see two patients of similar age and health have very different outcomes purely due to blood type compatibility. That inequity is what this universal kidney research is trying to address.
What Is a “Universal” Kidney?
A “universal” kidney is not a magical organ that every immune system automatically loves. Instead, it’s a donor kidney that’s been treated so its surface no longer loudly announces, “I am type A” or “I am type B” to the recipient’s immune system.
To understand this, it helps to know that blood types are determined by sugar molecules (antigens) on the surface of red blood cells—and similar markers appear on the cells lining blood vessels inside organs like the kidney.
- Normal state: A kidney from a type A donor has A antigens on its blood vessels.
- Mismatch risk: If a type B recipient receives that kidney, their immune system sees those A antigens as foreign.
- Universal goal: Remove or mask the A and B antigens so the kidney looks closer to type O (which is generally considered a “universal” donor type).

How Scientists Are Creating Universal Kidneys
The basic idea is elegant: run special enzymes through the kidney to remove the sugars that define blood type. The practice is technically demanding, and research teams have spent years refining the process so it doesn’t damage the organ.
Step-by-step: From Donor Kidney to “Universal” Organ
- Ex vivo perfusion:
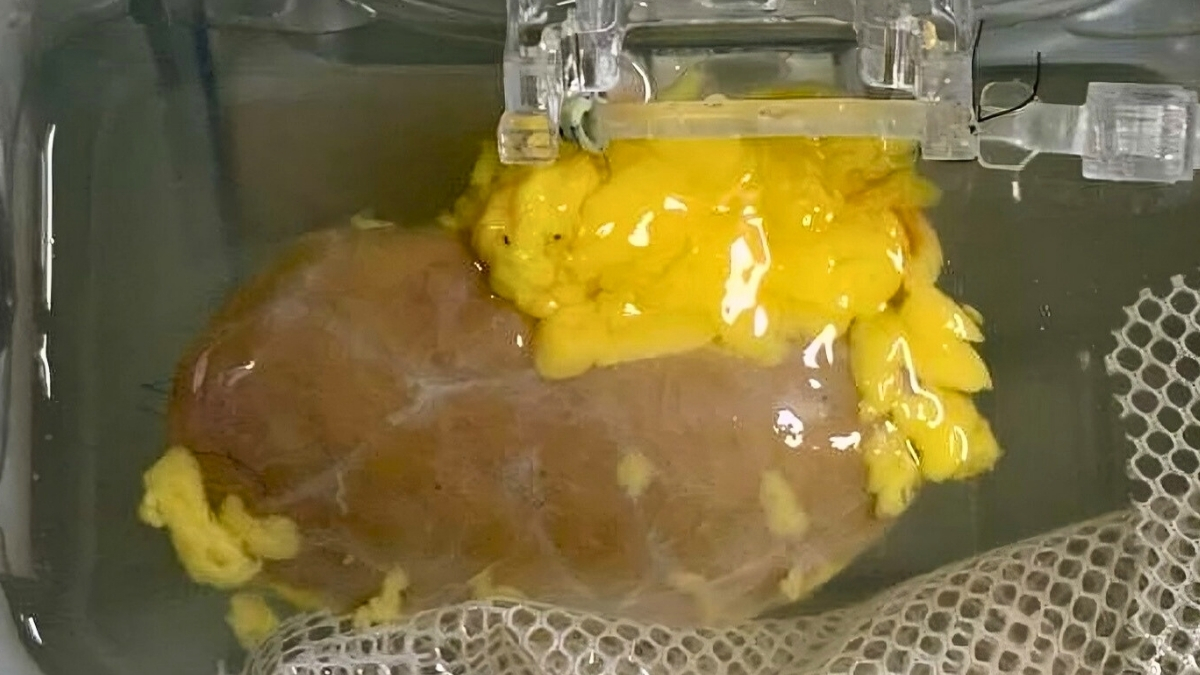
The kidney is connected to a machine that pumps warm, oxygen-rich solution through its blood vessels—keeping cells alive outside the body.
- Enzyme treatment:
Researchers add carefully chosen enzymes that cut off A or B blood group sugars from the vessel walls inside the kidney.
- Rinse and test:
The organ is flushed and then tested to confirm that blood-type antigens have been dramatically reduced or removed.
- Compatibility checks:
Scientists simulate contact with a different blood type in the lab to see how aggressively immune cells react.
- Transplant trials (carefully monitored):
Once safety thresholds are met, these kidneys can be transplanted in tightly controlled clinical trials with intense follow-up.
“We’re essentially washing away the blood-type identity from the kidney’s blood vessels. Early studies show this can dramatically reduce the immediate immune attack you’d expect from a mismatched transplant.”
— Lead researcher involved in universal kidney development

What Does the Latest Evidence Show?
As of early 2026, universal kidney research is still largely in the experimental and early clinical trial stages. Much of what we know comes from:
- Preclinical studies on kidneys that were not suitable for transplant.
- Laboratory tests exposing treated organs to mismatched blood.
- Initial, highly supervised transplants in select patients.
Early findings reported in peer-reviewed transplant and immunology journals suggest:
- Enzyme treatment can remove a large majority of A/B antigens from the kidney’s blood vessels.
- In lab tests, this significantly reduces the level of instant immune reaction you’d normally see with a mismatch.
- Short-term kidney function after experimental procedures can be comparable to standard transplants, though long-term data are still limited.
Most experts emphasize that this breakthrough will likely roll out in carefully monitored stages, starting with patients for whom standard options are very limited, such as those who are highly sensitized or have particularly rare blood types.
How Universal Kidneys Could Change Transplant Waiting Lists
If universal kidney techniques prove safe and effective at scale, the impact on transplant systems could be substantial. The core benefit is flexibility: organs could be allocated to the patients who need them most, without being blocked by blood type.
Potential Benefits
- Shorter wait times: Particularly for patients with blood types that currently wait longer.
- More equitable access: Communities that are overrepresented in certain blood groups could see fairer access to transplants.
- Less organ waste: Fewer suitable kidneys would be discarded or underused due to blood type restrictions.
- Improved paired donation chains: Living-donor kidney exchanges could become more flexible and efficient.

That said, universal kidneys are not a cure-all. Systems-level issues—like organ donation rates, geographic disparities, and access to specialized transplant centers—will still matter just as much.
Limits, Risks, and What We Still Don’t Know
It’s understandable to feel hopeful when you hear terms like “universal” and “breakthrough.” At the same time, managing expectations is crucial—especially when your health, or a loved one’s, is on the line.
Key Unknowns
- Long-term rejection: We don’t yet know how these treated kidneys will fare 5, 10, or 15 years after transplant.
- Subtle immune responses: Even with blood-type antigens removed, the immune system may still react to other markers.
- Cost and access: Perfusion machines, enzymes, and trained staff are expensive; not all hospitals will have these tools immediately.
- Regulatory pathways: Different countries will approve and adopt this technology at different speeds.
Clinicians will also need to track any unexpected complications unique to enzyme-treated organs. Until large-scale data are available, universal kidneys will remain an option offered primarily in specialized centers and within structured research protocols.
What This Means If You’re Waiting for a Kidney
If you’re currently on a kidney transplant waiting list, you may be wondering how—if at all—this affects your own timeline. For now, universal kidneys are not widely available, but the research is shaping how doctors think about future options for patients like you.
Practical Steps You Can Take Now
- Ask your transplant team about ongoing trials.
Large transplant centers sometimes participate in early-phase studies. They can tell you whether any universal kidney research is underway and who might qualify.
- Keep your overall health as strong as possible.
Whether you receive a standard or universal kidney in the future, better heart health, good nutrition, and consistent dialysis care improve your chances of a safe surgery and strong recovery.
- Discuss living donation and paired exchanges.
These options are proven today and may get even more powerful when combined with universal kidney techniques.
- Stay informed—but skeptical of hype.
Look for information from recognized transplant centers, government health agencies, and peer-reviewed journals rather than headlines alone.

A Real-World Scenario: When Blood Type Gets in the Way
Consider the experience—based on common patterns in transplant clinics—of a middle-aged patient with type B blood. Despite doing “everything right” on dialysis and staying active on the waiting list, their wait time stretches far longer than a neighbor with type O or A.
In many programs, type B patients can face significantly longer waits because there are fewer compatible kidneys and certain donor populations are underrepresented. A universal kidney approach wouldn’t change their medical history, but it could change how quickly a suitable organ reaches them:
- A donated kidney from a type A person could be enzyme-treated to remove A antigens.
- That same kidney might then be safely offered to the type B patient.
- The result: fewer months or years stuck in limbo on dialysis.
“When you see a patient finally get the call after years of waiting, it’s life-changing. Techniques that can safely expand the donor pool mean we may someday make those calls sooner—and to more people who’ve been overlooked by the current system.”
— Senior transplant coordinator
How Experts See the Future of Universal Organs
Transplant specialists generally see universal kidneys as part of a broader movement toward more personalized and more flexible transplantation. Alongside this work, scientists are:
- Exploring gene editing to reduce organ immunogenicity.
- Testing xenotransplantation (organs from animals, like genetically modified pigs).
- Developing better immunosuppressive drugs with fewer side effects.
- Investigating bioengineered and 3D-printed tissues, though these remain further from routine use.
Many experts predict a future where kidneys are not just matched by blood type, but by deeper immune signatures, genetics, and even lifestyle factors—with universal kidney techniques serving as a powerful stepping stone.
Staying Hopeful, Grounded, and Informed
Universal kidney research reflects some of the best of modern medicine: long, careful work aimed at turning a simple, humane idea—“make more organs usable for more people”—into reality. It’s not a cure for kidney disease, and it won’t erase the need for donors, but it may help ensure that fewer precious organs go unused and fewer patients wait in vain.
If you’re a patient, caregiver, or simply someone who cares about the future of transplant medicine, you can:
- Register as an organ donor and encourage others to do the same.
- Follow updates from reputable sources like national transplant networks and academic medical centers.
- Talk with your care team about how emerging research might intersect with your own treatment plan.
Progress in medicine often feels slow from the outside, especially when you’re waiting. But each incremental study moves us closer to a world where blood type is less of a barrier, and a safe, life-saving kidney is within reach for more people, more of the time.
