Nipah Virus in India: Why Texans Are Watching and What You Can Safely Do Now
When news breaks about a deadly virus in another part of the world, it’s natural to wonder what it means for you and your family. With confirmed Nipah virus cases recently reported in India and public health alerts in nearby countries like Thailand, many Texans are asking a simple, anxious question: “Should we be worried here in Texas?”
The short answer, based on current data as of February 8, 2026, is that the risk to people in Texas is very low. Still, it’s worth understanding what Nipah virus is, why it’s taken seriously by global health agencies, and how our own Texas Department of State Health Services (DSHS) fits into the picture.
This guide walks you through the facts, what experts are watching, how Texan health authorities prepare for threats like Nipah, and what practical steps you can take to stay informed without feeling overwhelmed.

What Is Nipah Virus, in Plain Language?
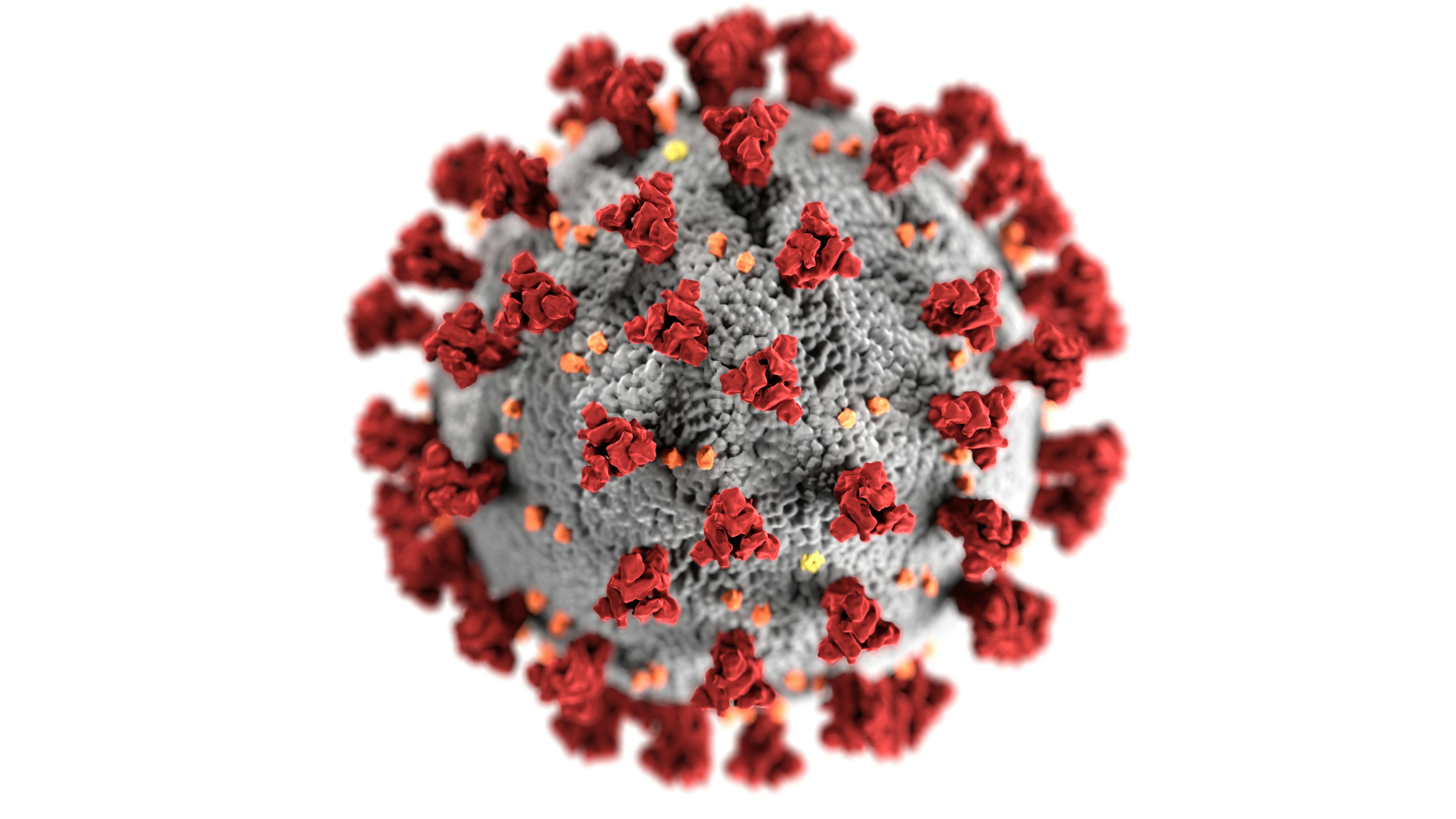
Nipah virus is a zoonotic virus—meaning it jumps from animals to humans—first identified in 1998–1999 during an outbreak in Malaysia and Singapore. It belongs to the Paramyxoviridae family, which includes viruses that can cause respiratory and neurological disease.
Scientists have learned that fruit bats, particularly those in the Pteropus genus, serve as the main natural reservoir. From bats, the virus can sometimes reach humans directly or through other animals such as pigs.
According to the World Health Organization (WHO) and research published in journals such as The Lancet Infectious Diseases, Nipah infection can range from mild respiratory illness to severe brain swelling (encephalitis). There is no licensed vaccine or specific antiviral treatment yet, so prevention and outbreak control rely heavily on rapid detection, isolation, and supportive medical care.
What’s Happening in India Right Now?
As of early February 2026, health authorities in India—particularly in the state of West Bengal—have confirmed several Nipah virus cases. Neighboring countries like Thailand have put their disease control agencies on high alert due to regional travel and shared bat populations.
Indian public health teams, in coordination with WHO and local epidemiologists, are:
- Tracing and monitoring close contacts of confirmed cases
- Restricting movement in affected localities when needed
- Testing suspected cases quickly with specialized labs
- Advising the public to avoid likely exposure sources, such as raw date palm sap or close contact with sick animals
“Nipah outbreaks tend to be tightly clustered in time and space. Early detection, strong local public health systems, and rapid communication are what prevent a local outbreak from becoming an international emergency.”
How Much Risk Does Nipah Pose to Texas Right Now?
Based on information available as of February 8, 2026, the Texas Department of State Health Services (DSHS) considers the risk of Nipah to Texans to be very low. There are several reasons for this:
- Geographic separation: The current Nipah activity is localized to specific regions in India, thousands of miles away from Texas.
- No local animal reservoir identified: The particular fruit bat species associated with Nipah in South Asia are not known to circulate in Texas in the same way.
- No travel-related cases reported in the U.S. at this time: U.S. Centers for Disease Control and Prevention (CDC) and state health departments monitor for unusual severe infections in travelers; no Nipah cases have been detected in Texas.
- Strong surveillance systems: Texas participates in national and global infectious disease surveillance networks that flag high-consequence pathogens.
How Nipah Spreads—and How It’s Different from COVID-19
When you hear “new virus,” it’s easy to think back to early COVID-19. Nipah behaves differently in several important ways.
Ways Nipah Can Spread
- Animal-to-human: Contact with infected bats or pigs, or with their bodily fluids (urine, saliva, or partially eaten fruit).
- Human-to-human: Close contact with the body fluids of an infected person, particularly in households or health care settings.
- Foodborne route: Drinking raw date palm sap that bats have contaminated (primarily an issue in some regions of South Asia).
Key Differences from COVID-19
- Not as easily airborne: Unlike SARS-CoV-2, there is currently no evidence of sustained, widespread transmission through small aerosol particles over long distances in everyday community settings.
- Outbreak pattern: Nipah outbreaks have historically been small and focused, not global waves affecting millions simultaneously.
- Known animal source: We understand more about its wildlife reservoir, which helps target prevention.
Nipah Symptoms: What Do Doctors Look For?
For people in affected regions or close contacts of known cases, clinicians watch for a combination of symptoms that can appear 4–14 days after exposure (sometimes longer in rare cases).
- Fever and headache
- Muscle aches and fatigue
- Cough, sore throat, and breathing difficulties
- Confusion, disorientation, or sudden behavior changes
- Seizures or coma in severe cases due to encephalitis
In Texas, the chance that these symptoms are caused by Nipah is currently extremely low. Much more common causes include influenza, COVID-19, RSV, and other respiratory or neurological infections. However, doctors stay alert for unusual patterns, especially in travelers returning from known outbreak areas.
What Is Texas DSHS Doing Behind the Scenes?
Even when the public risk is low, agencies like Texas DSHS do a lot of quiet, unglamorous work to stay ready for emerging infections.
Activities typically include:
- Surveillance: Reviewing reports of severe, unexplained illness from hospitals and labs.
- Coordination with CDC: Sharing data and receiving technical guidance on when special testing is needed.
- Laboratory readiness: Ensuring that public health labs know how to safely handle and ship samples to federal reference labs if Nipah is suspected.
- Healthcare provider alerts: Updating clinicians about what to look for in very specific situations (such as recent travel to an outbreak zone plus compatible symptoms).
“Most of the time, preparedness feels invisible—and that’s exactly the point. When systems work, the public sees calm, not chaos.”
Practical Steps Texans Can Take Right Now
While you can’t personally control a Nipah outbreak in another country, you can control how you respond to the news. Here are balanced, science-based steps you can take.
1. Choose Reliable Information Sources
- Follow updates from Texas DSHS.
- Check the CDC and WHO for global perspectives.
- Be cautious with social media posts that lack sources or sound overly dramatic.
2. If You’re Traveling
If you or your loved ones are traveling to South Asia, especially regions with Nipah activity:
- Review CDC travel advisories for the destination.
- Avoid contact with bats, pigs, and other animals in affected areas.
- Do not drink raw date palm sap or consume fruit that may have been partially eaten by animals.
- Practice strong hand hygiene and routine respiratory etiquette.
3. Keep Your General Health Defenses Strong
Even though specific Nipah prevention isn’t necessary for everyday life in Texas right now, the habits that protect you from many infections still matter:
- Stay current on recommended vaccines (flu, COVID-19, and others your clinician suggests).
- Wash hands frequently, especially before eating and after being in public spaces.
- Stay home when you’re sick when feasible, to protect others.

A Realistic Scenario: How a Concerned Texan Responds
Consider “Maria,” a Houston resident with family in Kolkata, India. When she hears about Nipah cases in West Bengal, her first response is fear—especially for her elderly parents.
Instead of spiraling into worst-case scenarios, Maria:
- Checks the WHO and India’s Ministry of Health websites for localized updates.
- Asks her parents’ doctor about practical precautions (avoiding crowded hospitals unless needed, good hand hygiene, and steering clear of raw date palm sap).
- Subscribes to Texas DSHS email alerts to stay abreast of any change in risk levels at home.
- Limits doomscrolling and focuses on what she can control: communication, preparation, and emotional support.
Maria can’t eliminate all risk—for her family or herself—but she can replace helplessness with informed, measured action. That’s the same opportunity you have.
Myths vs. Facts About Nipah for Texans
- Myth: “Nipah is the next COVID-19 for the U.S.”
Fact: Current evidence does not support that. Outbreaks have been localized and linked to specific animal and environmental exposures, with no sign of widespread international transmission. - Myth: “Any fever after a flight from Asia must be Nipah.”
Fact: Much more common infections (like flu or COVID-19) are far more likely. Still, travelers with high fever or severe symptoms should seek medical care and mention their travel history. - Myth: “There’s nothing anyone can do about viruses like this.”
Fact: Public health measures—contact tracing, travel guidance, lab surveillance, and infection control practices—have already prevented many localized outbreaks from spreading widely.

Before vs. After: Understanding Nipah Risk in Texas
It can help to compare how you might feel about the outbreak before having accurate information and after you’ve learned the facts.
| Before | After |
|---|---|
| “Nipah is in the news; I’m afraid it’s coming here next.” | “Outbreaks are localized in India; current risk in Texas is very low, but experts are watching.” |
| Constantly refreshing social media for rumors. | Checking DSHS, CDC, and WHO for periodic, evidence-based updates. |
| Feeling helpless and overwhelmed. | Focusing on practical steps: healthy habits, travel precautions, and staying informed. |
Where to Get Trusted Updates on Nipah and Other Emerging Viruses
For Texans who want to keep a grounded, science-based view of Nipah and other emerging infections, these resources are a strong starting point:
- Texas Department of State Health Services (DSHS) – State-level alerts, guidance, and contact information.
- CDC: Nipah Virus (NiV) – Technical fact sheets, FAQs, and updates for clinicians and the public.
- World Health Organization: Nipah Virus Infection – Global situation reports and technical guidance.
- Peer-reviewed articles in journals such as The Lancet Infectious Diseases and Clinical Infectious Diseases for deeper scientific reading.
Staying Calm, Prepared, and Compassionate
It’s understandable to feel uneasy when you hear about a deadly virus on the other side of the world. But as of now, Texans face a very low direct risk from the Nipah outbreak in India. Public health professionals in India, the broader region, and here in the U.S. are actively monitoring and responding.
Your role isn’t to carry the weight of global disease control on your shoulders. Your role is to:
- Stay informed from trustworthy sources
- Support reasonable public health measures when they’re recommended
- Maintain healthy daily habits that protect you and those around you
- Avoid stigmatizing people from affected regions—viruses exploit fear and division
If you’d like tailored guidance—especially around travel or complex medical conditions—consider reaching out to your healthcare provider or a travel medicine clinic. A short conversation can replace days of worry with a clear, personalized plan.
Take a moment now to bookmark the Texas DSHS, CDC, or WHO pages, and commit to checking them if you see alarming headlines. That simple step turns you from a passive consumer of anxiety into an active, informed partner in public health.
