Ohio’s First Pediatric Flu Death This Season: What Parents Need to Know Now
News that a Greene County teen has become Ohio’s first pediatric flu death of the season is both heartbreaking and unsettling, especially as cases rise between December and February. For many parents, it raises scary questions: How worried should I be? Is my child safe at school? Am I doing enough to protect my family?
This article walks you through what this tragic report actually means, how flu affects children, and the most effective, science-backed ways to lower your child’s risk—without panic, guilt, or false promises.
What This Pediatric Flu Death Means for Families in Ohio
According to state health officials, Ohio typically reports one to seven flu-related pediatric deaths each season. Even one death is too many for the families involved, but in the context of millions of children, these events remain relatively rare.
Flu season in Ohio usually:
- Starts to rise in November
- Peaks between December and February
- Can linger into early spring, depending on the circulating strains
“Pediatric flu deaths are devastating, but they’re also a reminder that influenza is not ‘just a bad cold.’ The good news is that we have tools—vaccination, early treatment, and prevention—that can significantly reduce the risk.”
— Board-certified pediatric infectious disease specialist
This first reported death doesn’t mean every child is in immediate danger, but it is a signal that flu is actively circulating and that now is the time to tighten up prevention.
Why Influenza Can Be So Serious for Children
Influenza is a respiratory virus that infects the nose, throat, and sometimes the lungs. In children, it can lead to:
- Pneumonia (viral or bacterial)
- Worsening of chronic conditions like asthma, diabetes, or heart disease
- Dehydration from poor intake and high fevers
- Inflammatory complications such as encephalitis (brain inflammation)
Even previously healthy kids can become very ill, though the highest risks are in:
- Children under 5, especially under 2
- Kids with asthma or other lung conditions
- Those with heart disease, neurologic conditions, or weakened immune systems

How to Protect Your Child This Flu Season
No strategy can guarantee your child won’t get the flu, but you can significantly lower risk and severity with layered protection.
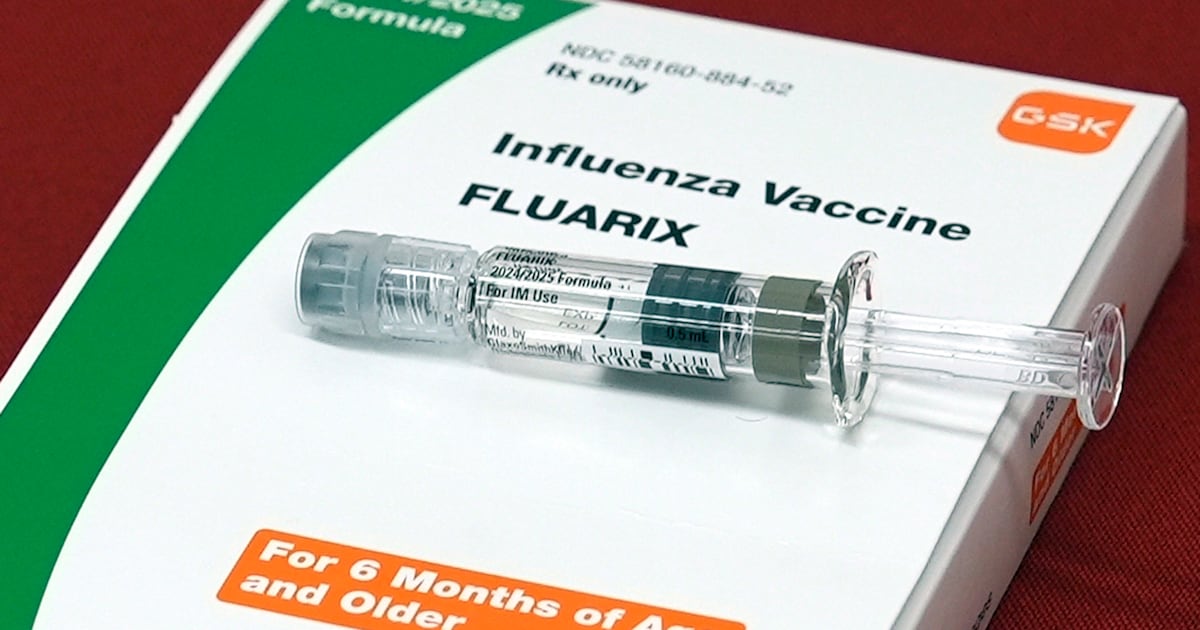
1. Vaccination: Your Strongest Single Tool
The CDC and American Academy of Pediatrics recommend a yearly flu vaccine for everyone 6 months and older, unless there’s a specific medical reason not to.
- It’s best to vaccinate in the fall, but late vaccination is still worthwhile if flu is circulating.
- Most kids develop good protection about 2 weeks after the shot.
- While not perfect, the vaccine consistently reduces the risk of severe illness, hospitalization, and death in children.
2. Everyday Habits That Really Do Help
Simple, consistent habits add a meaningful layer of protection:
- Hand hygiene: Teach kids to wash for 20 seconds with soap and water, or use sanitizer with at least 60% alcohol.
- Stay home when sick: Keep kids with fever, deep cough, or body aches out of school and activities.
- Cover coughs and sneezes: Into the elbow or a tissue, followed by hand washing.
- Clean high-touch surfaces: Doorknobs, light switches, phones, and shared devices.
- Improve ventilation: When possible, open windows slightly or use air filtration, especially with guests.
3. Consider Extra Precautions in High-Risk Families
If your child or a household member is at higher risk for complications:
- Talk with your clinician about early antiviral treatment (like oseltamivir) if flu is suspected.
- Ask schools or caregivers to notify you quickly if there’s a cluster of illness in your child’s classroom.
- During peak weeks, you may choose to limit crowded indoor events, especially if vaccination is incomplete.
Flu Symptoms in Kids: When to Worry and Seek Help
Flu often starts suddenly. Early symptoms can look like many other viruses, but some patterns are more typical for influenza.
Common Flu Symptoms
- High fever and chills
- Body aches, headaches
- Dry cough and sore throat
- Fatigue, wanting to lie down or sleep more
- Sometimes nausea, vomiting, or diarrhea (more common in kids than adults)
Emergency Warning Signs in Children
Seek urgent or emergency care immediately (call your local emergency number if needed) if your child has:
- Fast, difficult, or labored breathing
- Blue, gray, or very pale lips or face
- Chest pain or ribs pulling in with each breath
- Severe muscle pain (refusal to walk or move)
- Not drinking or urinating very little (signs of dehydration)
- Seizures, confusion, or not waking up/ interacting as usual
- Flu that seems to get better then suddenly worsens with renewed fever and cough
A Real-Life Scenario: From Mild Illness to ER Visit
A family I once worked with had a 13-year-old who came down with what seemed like a typical winter bug—fever, fatigue, body aches. They kept him home, gave fluids, and monitored closely.
On day two, his breathing seemed slightly faster, but he was still talking and watching TV. Overnight, he developed:
- Fast breathing and a feeling of “can’t catch my breath”
- New chest pain with cough
- Extreme fatigue—barely responding to questions
The parents trusted their instincts and went straight to the emergency department. He was diagnosed with influenza and pneumonia, required oxygen, and was admitted for several days—but he recovered fully.
Their decision to seek care when “something didn’t look right” likely prevented things from becoming much worse. Knowing the warning signs—and acting on them—can be lifesaving.
What a Difference Prevention Can Make
We can’t see alternate timelines for an individual child, but population data give us a “before and after” picture of what happens when flu vaccination and early care are widely used.

Large studies from the CDC and academic centers consistently show that flu vaccination in children is associated with:
- Lower risk of flu-related pediatric deaths
- Fewer hospitalizations and ICU stays
- Shorter duration and milder severity of illness in many cases
Common Barriers Parents Face—and How to Move Past Them
Even when parents want to do everything they can, real-life barriers get in the way. Here are some you might recognize.
“We Meant to Get the Flu Shot, But Time Got Away from Us”
- Look for evening or weekend clinics at pharmacies or urgent care centers.
- Ask your pediatrician if they offer walk-in vaccination hours.
- Pair it with another errand—like picking up groceries or prescriptions—so it feels less like an extra trip.
“I’m Worried About Side Effects”
Most side effects from the flu shot are mild—sore arm, low fever, or fatigue for a day or two. Severe reactions are very rare. If your child has a history of reactions or allergies, talk with their clinician about the safest approach.
“We’re Not Sure If It’s Flu, COVID-19, or Something Else”
Symptoms can overlap. If your child is quite ill, has risk factors, or lives with high-risk family members, ask about testing. Knowing whether it’s flu can open the door to early antiviral treatment.
What the Science and Experts Say
Multiple high-quality studies and national data sources support the strategies discussed here:
- The U.S. Centers for Disease Control and Prevention (CDC) tracks flu activity and pediatric deaths each season, showing that deaths occur even in otherwise healthy children.
- Research summarized by the CDC indicates that flu vaccination significantly reduces the risk of severe outcomes in kids, including ICU admission and death.
- The American Academy of Pediatrics provides detailed guidance on recognizing flu symptoms, caring for sick children, and when to seek emergency care.
Moving Forward: Calm, Informed, and Prepared
Hearing about a pediatric flu death in Greene County is deeply unsettling, especially when you picture your own child. It’s normal to feel a mix of fear, sadness, and urgency.
While we can’t erase risk completely, we can stack the odds in our children’s favor:
- Stay up to date on flu vaccination for your family.
- Practice and model everyday prevention habits.
- Know the warning signs that mean it’s time to seek urgent care.
- Reach out to your child’s clinician when you’re unsure—questions are part of good parenting, not a burden.
If this news story has been weighing on you, consider taking one small step today—checking your child’s vaccination status, restocking fever medicine and thermometers, or saving your pediatrician’s after-hours number in your phone. Those quiet, practical moves are how you turn worry into protection.
Your concern is a sign of how deeply you care. With informed choices and timely action, most children who get the flu recover fully—and your preparation can make that path safer and smoother.
