Nipah Virus Outbreak in India: What Travelers and Families Really Need to Know Right Now
Amid a new Nipah virus outbreak in West Bengal, India, and heightened screening at airports across Southeast Asia, it’s completely understandable to feel uneasy. Nipah virus is rare but serious, with no specific cure, and headlines about “deadly outbreaks” can make it hard to know what to believe—or how worried you should be.
This guide brings together the latest information from global health agencies and recent reports (as of late January 2026) to explain what Nipah virus is, how it spreads, what this current outbreak means, and, most importantly, what practical steps you can take to protect yourself and your family without giving in to panic.

“Nipah virus is a zoonotic virus that causes severe disease in animals and humans. Although outbreaks are relatively rare, they require rapid detection and strong public health response.”
— World Health Organization (WHO)
Why the Current Nipah Virus Outbreak Matters
Nipah virus outbreaks have occurred almost every year somewhere in South Asia over the past decade, especially in Bangladesh and India. The latest confirmed cases in West Bengal have prompted airport health screenings in parts of Southeast Asia, including Thailand, because:
- Case fatality can be high (often 40–75% in past outbreaks, depending on available care).
- The virus can spread from animals to humans and between humans through close contact.
- There is no specific antiviral drug or widely available vaccine yet, so prevention and supportive care are crucial.
- Travel can move infected people quickly before symptoms fully develop, requiring careful screening and tracing.
At the same time, it’s important to keep perspective: Nipah is not spreading worldwide like COVID-19. Outbreaks have been localized, and strong public health measures—early detection, isolation, and contact tracing—have repeatedly stopped chains of transmission.
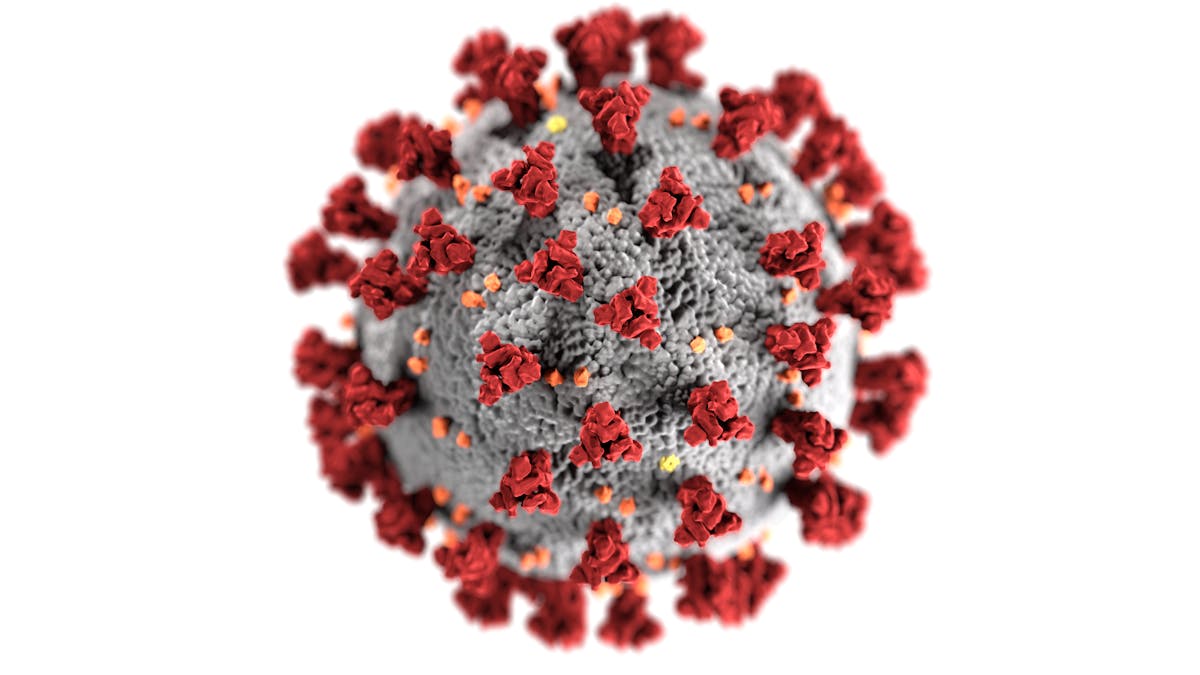
What Is Nipah Virus and Where Does It Come From?
Nipah virus (NiV) is a zoonotic virus, meaning it originally circulates in animals and can jump to humans. It was first identified during an outbreak among pig farmers in Malaysia in 1998–1999. Since then, outbreaks have occurred mainly in:
- Bangladesh
- India (including Kerala and now West Bengal)
- Occasionally other parts of South and Southeast Asia where the natural host lives
The natural reservoir of Nipah virus is fruit bats of the genus Pteropus, often called flying foxes. These bats can carry the virus without appearing sick. The virus can pass from bats to:
- Humans (for example, through consuming raw date palm sap contaminated with bat secretions)
- Domestic animals like pigs, which then infect humans through close contact

“Spillover events from animals to humans usually happen in very specific settings—such as consuming contaminated food or prolonged close contact with infected animals. They are not random, everyday events for the general public.”
— Infectious disease epidemiologist, South Asia (case discussion, anonymized)
Symptoms of Nipah Virus: What to Watch For
Nipah virus infection can range from mild illness to rapidly progressive, life-threatening disease. The incubation period (time from exposure to symptoms) is typically 4–14 days, but longer periods up to 45 days have been reported in rare cases.
Common early symptoms include:
- Fever
- Headache
- Muscle pain
- Sore throat
- Fatigue and general malaise
As the illness progresses, more serious symptoms can develop:
- Severe respiratory distress (shortness of breath, cough)
- Confusion, disorientation, or changes in behavior
- Drowsiness or difficulty staying awake
- Seizures
- Encephalitis (inflammation of the brain), which can lead to coma
Nipah symptoms overlap with many other infections, including COVID-19, flu, and other viral encephalitides. That’s why, in areas where Nipah is circulating, travel history, exposure history, and contact tracing are so important for correct diagnosis.
How Nipah Virus Spreads (and How It Doesn’t)
Understanding transmission is crucial to lowering your risk without overreacting. Based on WHO, CDC, and regional health authority data, Nipah spreads primarily through:
- Animal-to-human spread
- Exposure to fruit bats or their secretions (urine, saliva, feces).
- Consumption of fresh date palm sap or fruit contaminated with bat secretions—this has been a major route in Bangladesh.
- Close contact with infected pigs or other animals (handling, slaughtering, caring for sick animals).
- Human-to-human spread
- Prolonged, close contact with the body fluids of an infected person (respiratory droplets, saliva, urine, blood).
- Exposure during caregiving, especially without proper protective equipment.
- In some outbreaks, spread has occurred within families and in healthcare facilities.
There is currently no evidence that Nipah virus spreads efficiently through casual community contact, shopping in markets, or brief contact in public spaces. It is not known to be airborne in the same way as measles or as easily transmissible as seasonal flu.

The West Bengal Outbreak and Airport Screenings: What’s Happening Now
In the latest outbreak in West Bengal, Indian health officials have confirmed Nipah cases and are implementing containment measures such as:
- Isolating confirmed and suspected cases in designated facilities.
- Tracing and monitoring close contacts for symptoms.
- Temporarily restricting movement in high-risk zones if needed.
- Reinforcing infection prevention protocols in hospitals.
Neighboring countries, including Thailand and some others in Southeast Asia, have responded by:
- Setting up health screening checkpoints at airports for passengers arriving from affected regions.
- Using thermal scanners and health questionnaires to identify potentially ill travelers.
- Preparing isolation areas and rapid testing pathways for suspected cases.
These steps are designed to catch cases early and prevent the virus from seeding new outbreaks in other countries. They can be inconvenient for travelers, but they are part of a proven playbook used in past Nipah outbreaks and during other emerging infections.
“Border health measures—when focused and time-limited—can slow the spread of high-risk pathogens and buy health systems valuable time to respond.”
— Regional public health official, Southeast Asia (policy briefing, anonymized)
Who Is Most at Risk from Nipah Virus?
While anyone in close contact with an infected person or animal can be at risk, past outbreaks and current data suggest higher risk for:
- Healthcare workers caring for Nipah patients, especially if personal protective equipment (PPE) is inadequate or inconsistently used.
- Family members and caregivers who provide close, hands-on care at home or share living spaces with infected individuals.
- Farmers and animal handlers in regions where Nipah is known to circulate, particularly those working with pigs or exposed to bat habitats.
- People consuming raw date palm sap or unwashed fruit in endemic areas where bats feed.
Age and existing health conditions may influence the severity of disease, but the primary driver of risk is exposure intensity and type, not simply being in the same city or country.
Practical Prevention Steps: What You Can Do Right Now
While we don’t yet have a widely available Nipah vaccine, we do have effective behavioral and public health tools. Here are evidence-informed steps you can take, tailored to different situations.
For people living in or near affected areas
- Avoid raw date palm sap and unwashed fruit, especially if bats are known to feed in the trees.
- Wash hands frequently with soap and water or use alcohol-based sanitizer.
- Avoid close physical contact (kissing, sharing utensils, sleeping in the same bed) with anyone who is acutely ill with fever and neurological or respiratory symptoms.
- Follow local public health advice, including any movement restrictions or guidance on school, work, or community events.
For travelers
- Check WHO and your country’s travel health advisory (e.g., CDC) before departure.
- Be honest on health declaration forms and temperature screenings; they protect you and others.
- Consider wearing a well-fitted mask in crowded indoor spaces in affected regions, especially around visibly unwell people.
- Seek medical advice promptly if you develop symptoms during or after travel and mention your travel history.
For healthcare workers and caregivers
- Use appropriate PPE (mask or respirator per local protocol, eye protection, gloves, gown) when caring for suspected or confirmed Nipah patients.
- Practice strict hand hygiene before and after every patient contact.
- Follow facility protocols for isolation, waste disposal, and environmental cleaning.
- Report any unprotected exposures promptly to occupational health services.

Treatment, Care, and Experimental Options
There is currently no specific antiviral drug that is universally recommended and approved solely for Nipah virus in humans. Treatment is mainly:
- Supportive care—maintaining breathing, blood pressure, and organ function.
- Intensive care for severe encephalitis or respiratory distress.
- Symptom management (fever control, seizure treatment, hydration, nutrition).
Several experimental approaches—such as monoclonal antibodies targeting henipaviruses and repurposed antivirals—are under study in clinical and preclinical settings. Some have shown promise in animal models and limited human use under emergency protocols, but they are not yet widely available or proven cures.
From a practical standpoint, the best “treatment” remains early recognition, rapid medical evaluation, and high-quality supportive care, which can improve survival compared to delayed or limited care.
“We must be very careful not to oversell experimental therapies. For Nipah, the front line is still basic public health: finding cases quickly, supporting patients, and protecting healthcare workers and communities.”
— Infectious disease physician, India (clinical debrief, anonymized)
Vaccines and Research: What’s on the Horizon?
Nipah virus is classified by WHO as a priority pathogen because of its high mortality and pandemic potential. As a result, there is active global research into:
- Vaccine candidates, including:
- Viral vector vaccines (similar platforms to some COVID-19 vaccines).
- Subunit vaccines targeting the Nipah G (glycoprotein).
- mRNA-based approaches in early-stage development.
- Monoclonal antibodies designed to neutralize the virus, some of which have shown protective effects in animal studies and limited human use under emergency protocols.
- Improved diagnostics for quicker, more reliable detection in both humans and animals.
While these developments are encouraging, it is important not to assume that a widely available Nipah vaccine or specific treatment will arrive immediately. Public health measures and healthcare system preparedness remain the backbone of our response for now.

Common Challenges: Fear, Stigma, and Misinformation
Whenever a lethal virus makes headlines, three things tend to spread faster than the virus itself: fear, stigma, and misinformation. Nipah is no exception.
Some common challenges people face include:
- Overwhelming anxiety—worrying that every headache or cough is Nipah, especially if you live in or near affected regions.
- Blame and stigma—targeting certain communities, regions, or occupations (e.g., pig farmers, bat conservationists, travelers from certain countries).
- Rumors and unproven “cures”—herbal remedies, miracle supplements, or conspiracy theories spreading on social media.
Managing these challenges is just as important as managing the virus itself, because fear and stigma can keep people from seeking care early or cooperating with public health teams.
Putting Nipah in Context: Before and After Public Health Measures
It can be helpful to compare what Nipah looks like without versus with strong public health responses, based on previous outbreaks.

This “before and after” pattern underscores a key message: our actions matter. Early reporting of symptoms, honest sharing of travel and exposure history, and adherence to public health guidance can dramatically change the course of an outbreak.
Staying Informed and Prepared—Without Panic
Nipah virus is serious, and the new outbreak in India deserves attention. But attention does not have to mean alarm. Understanding how the virus behaves, how it spreads, and what health systems are doing right now can help you make calm, informed decisions.
Here’s a simple action plan you can start today:
- Check an official source (WHO, your national health ministry, or CDC) for current Nipah updates in your region.
- Review your habits: handwashing, avoiding close contact with the acutely ill, and food hygiene if you live in or visit affected areas.
- Talk with your family or travel group about what you’ll do if someone develops symptoms after travel.
- Support accurate information by sharing reputable articles and gently correcting misinformation when you see it.
Outbreaks will continue to happen in our interconnected world—but so will scientific progress, smarter health systems, and informed communities. By staying grounded in evidence and focusing on practical steps, you can protect yourself and contribute to a safer, more resilient response for everyone.
