Nipah Virus in India: What You Need to Know, How to Stay Safe, and Why Calm Preparedness Matters
News about a fresh Nipah virus outbreak in India can feel alarming—especially when you read that there is “no cure” and “epidemic potential.” If you live in India, have family there, or simply follow global health news, it’s completely natural to feel uneasy or overwhelmed.
In this article, we’ll break down what’s actually happening with the Nipah virus outbreak reported in West Bengal, how the virus spreads, what symptoms to watch for, and the evidence-based steps you can take to stay safe. The goal is not to fuel fear, but to replace it with calm, informed preparedness.
What Is Happening With Nipah Virus in India Right Now?
As of late January 2026, Indian health officials in the eastern state of West Bengal are responding to a cluster of confirmed Nipah virus (NiV) infections. Media reports, including LADbible and local outlets, cite at least five confirmed cases and active containment efforts. Because information can evolve quickly during outbreaks, it is important to rely on updated sources such as:
- India’s Ministry of Health and Family Welfare
- The National Centre for Disease Control (NCDC), India
- The World Health Organization (WHO)
- The US Centers for Disease Control and Prevention (CDC)
Officials typically respond to Nipah cases by tracing contacts, isolating suspected and confirmed cases, monitoring healthcare workers, and restricting movement in high-risk zones. These steps are similar to what has been done during previous Nipah events in India, such as in Kerala (2018, 2019, 2021, and 2023), and have been effective in limiting the size of outbreaks.
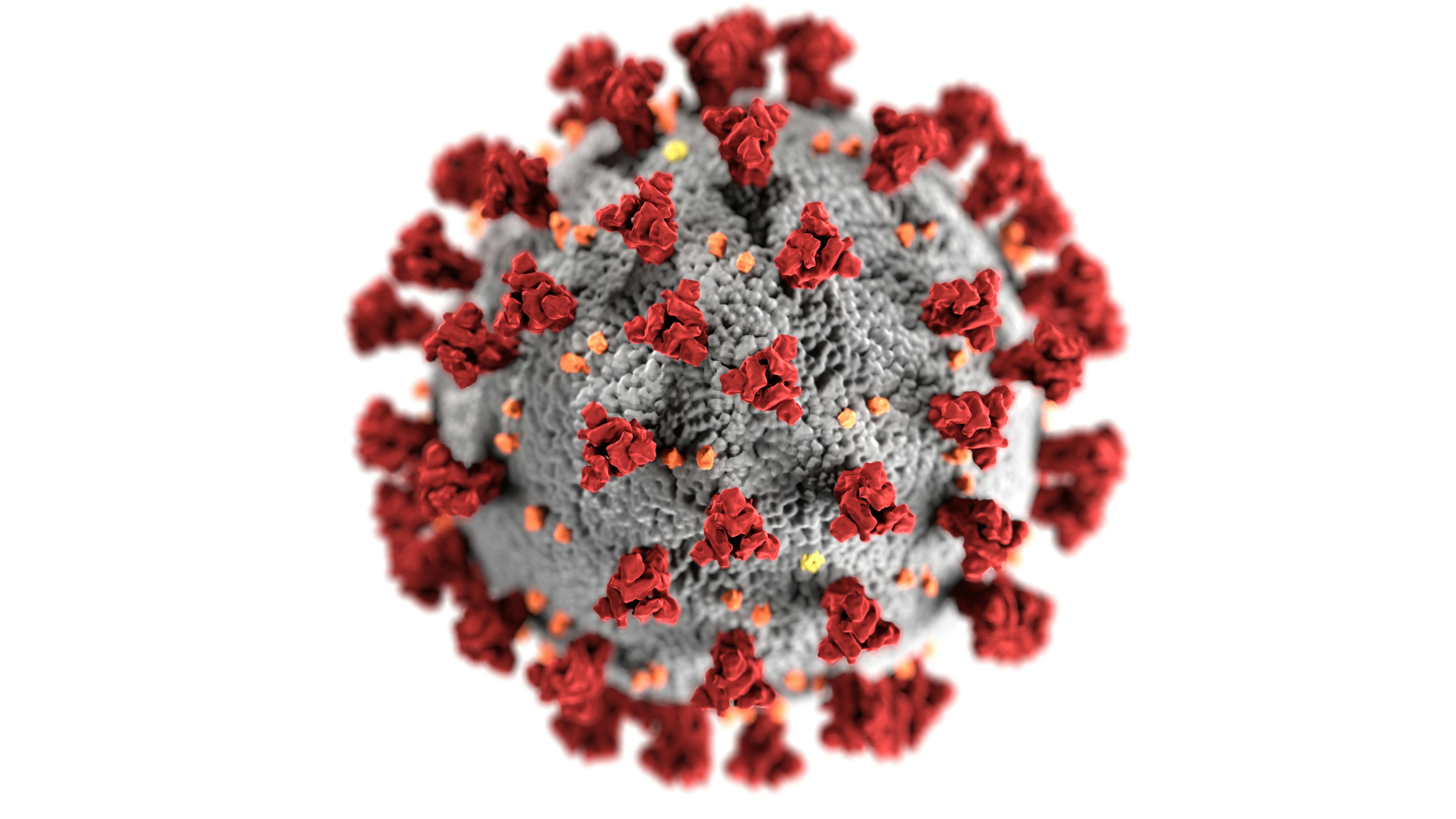
Nipah Virus 101: A Quick, Evidence-Based Overview
Nipah virus is a zoonotic virus (it jumps from animals to humans) first identified in 1998–1999 during an outbreak among pig farmers in Malaysia and Singapore. Since then, sporadic outbreaks have occurred in Bangladesh and India, mostly linked to fruit bats and contaminated food.
- Natural host: Fruit bats of the Pteropus genus (often called flying foxes).
- Transmission: From bats or other animals to humans, and in some outbreaks, person-to-person through close contact with bodily fluids.
- Illness range: From mild or no symptoms to severe respiratory illness and fatal encephalitis (brain inflammation).
- Case fatality rate: Historically 40–75% in some outbreaks, depending on care access and detection speed. Estimates vary.
- Treatment: No specific antiviral drug or licensed vaccine yet; care is largely supportive (managing symptoms and complications).
“Nipah virus infection is a zoonotic illness which can be transmitted to humans from animals, contaminated food or directly from person-to-person. The virus causes a range of illnesses… There are currently no licensed treatments or vaccines specific for Nipah virus infection.”
— World Health Organization (WHO) Nipah Virus Fact Sheet

How Nipah Virus Spreads: Key Routes of Transmission
Understanding how Nipah virus spreads is central to protecting yourself and your family. Based on past outbreaks and current WHO/CDC guidance, the main pathways are:
- Animal-to-human transmission
- Contact with infected bats, pigs, or their bodily fluids (saliva, urine, blood, or respiratory secretions).
- Consumption of food contaminated by bats, especially raw date palm sap or fruits partially eaten by bats.
- Human-to-human transmission
- Close, unprotected contact with an infected person’s bodily fluids (respiratory droplets, saliva, urine, or blood).
- Household caregiving and healthcare settings are the most common contexts for this kind of spread.
To date, casual community contact—like briefly passing someone on the street—has not been a typical driver of Nipah outbreaks. Most chains of transmission have involved prolonged, close contact, especially with very sick individuals.
Nipah Virus Symptoms: What to Watch For
Symptoms of Nipah virus usually appear between 4 and 14 days after exposure (the “incubation period”), though rare cases with longer incubation have been reported. Early symptoms can look like many other viral illnesses, which is why context—such as exposure to a confirmed case or outbreak area—matters.
- Early symptoms: Fever, headache, muscle pain, fatigue, sore throat.
- Progressive symptoms: Cough, difficulty breathing, chest discomfort.
- Severe symptoms: Disorientation, confusion, drowsiness, seizures, and in some cases, coma due to encephalitis (brain inflammation).
If you develop these symptoms and have:
- Been in a region with an active Nipah outbreak, or
- Had close contact with a suspected or confirmed Nipah patient, or
- Handled sick animals (especially pigs) in affected areas,
you should seek medical care immediately and inform healthcare workers about your possible exposure.
“When we caught one cluster early during a previous Nipah event, everyone who got supportive care quickly had a much better chance. The key was people not ignoring early, ‘simple’ symptoms in a high‑risk area.”
— Infectious disease physician, recounting a Nipah cluster response in India
Who Is Most at Risk During a Nipah Outbreak?
While anyone can, in theory, get infected, certain groups face higher risk, especially in an active outbreak zone:
- Family members and caregivers of infected patients without adequate protection.
- Healthcare workers in contact with suspected or confirmed Nipah cases without proper PPE.
- People who handle or consume raw date palm sap or fruits potentially contaminated by bats.
- Workers in pig farming or animal handling in affected regions, if the animal reservoir is involved.
For people outside outbreak areas, especially those in other Indian states or other countries, current risk remains very low, based on patterns from previous Nipah outbreaks. Most Nipah events have remained geographically limited thanks to rapid containment efforts.

Practical Steps to Protect Yourself and Your Family
Even without a specific vaccine or cure, there is a lot you can do to reduce your risk. The following measures draw on WHO and CDC recommendations, adapted for everyday life in affected regions:
1. Strengthen everyday hygiene
- Wash hands frequently with soap and water for at least 20 seconds, especially after caring for someone who is ill or visiting healthcare facilities.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Use alcohol-based hand sanitizer when soap and water are not available.
2. Avoid high‑risk foods and exposures
- Do not drink raw date palm sap in affected regions; drink only boiled or commercially processed drinks.
- Avoid eating fruits that appear partially eaten or contaminated by animals.
- Wash and peel fruits thoroughly before eating.
3. Practice safer caregiving
- If a family member has symptoms suggestive of Nipah and has a relevant exposure history, seek medical care promptly.
- Limit the number of caregivers; ideally one healthy adult provides care.
- Use masks, gloves, and, if possible, eye protection when dealing with bodily fluids.
- Wash bedding, clothes, and utensils of sick individuals separately with soap and hot water.
4. Follow public health guidance
- Cooperate with contact-tracing teams and provide accurate information.
- Respect movement restrictions or containment zones if implemented.
- Rely on official health department updates instead of unverified social media posts.
How Authorities Contain Nipah: What Happens Behind the Scenes
Nipah is listed by the WHO as a “priority disease” because of its epidemic potential, even though outbreaks are typically small. This designation pushes governments and global agencies to respond aggressively and quickly. Typical containment steps include:
- Case identification and isolation – Rapid testing, isolating suspected and confirmed cases in healthcare facilities or designated centers.
- Contact tracing – Identifying people who had close contact with cases, monitoring them for symptoms, and quarantining when needed.
- Infection prevention and control (IPC) in hospitals – Enforcing PPE use, safe waste disposal, and dedicated Nipah wards.
- Risk communication – Providing clear, frequent updates to the public to discourage rumors and panic.
- Animal and environmental investigations – Working with veterinary and wildlife experts to identify possible animal sources.
In previous Indian outbreaks, these strategies have limited Nipah’s spread to a relatively small number of cases compared with its theoretical epidemic potential.
Is There Really “No Cure”? What Treatment Looks Like
When headlines say “no cure” or “no vaccine,” they mean that there is currently no Nipah‑specific antiviral medication or fully approved human vaccine widely available as of early 2026. That does not mean nothing can be done.
In practice, patients benefit from:
- Careful monitoring of vital signs and neurological status.
- Supportive treatment like oxygen therapy, fluids, and management of seizures or brain swelling.
- Management of complications in intensive care units when needed.
Experimental therapies and vaccine candidates have been under development, often supported by organizations such as the Coalition for Epidemic Preparedness Innovations (CEPI). Some have reached early human trials, but they are not yet standard of care or widely deployed in outbreak settings.
Common Myths About Nipah Virus (And the Facts)
In every outbreak, misinformation spreads faster than the virus itself. Here are a few myths already circulating, along with evidence‑based clarifications:
- Myth: “Everyone who gets Nipah dies.”
Fact: While Nipah has a high case fatality rate compared with many infections, not all patients die. Outcomes vary by outbreak and by how quickly supportive care is provided. - Myth: “Nipah spreads as easily as COVID‑19 through the air.”
Fact: Nipah primarily requires close contact with bodily fluids. It has not shown the same kind of widespread, sustained community transmission seen with highly airborne viruses. - Myth: “Home remedies can cure Nipah virus.”
Fact: No home remedy has been proven to cure Nipah. You can support your general health with rest, hydration, and nutrition, but medical care is essential. - Myth: “There is nothing we can do until a vaccine arrives.”
Fact: Hygiene measures, safe caregiving, food precautions, and strong public health responses are powerful tools we already have today.
Coping With Fear and Uncertainty During an Outbreak
Living through any outbreak can be emotionally draining. People in affected neighborhoods in West Bengal—and their families elsewhere—may feel anxious, angry, or helpless. These reactions are normal, but they don’t have to control your decisions.
A few strategies that can help:
- Limit doom‑scrolling: Check reliable updates once or twice a day instead of constantly refreshing social media.
- Create a simple plan: Decide in advance what you’ll do if someone in your home gets sick—where to seek care, who will accompany them, what to pack.
- Stay connected: Talk regularly with friends, family, and neighbors. Social support lowers stress.
- Care for your basics: Sleep, hydration, and regular meals aren’t luxuries—they’re your foundation for coping.
“In my experience, communities that stay informed without panicking—who focus on what they can control—tend to get through outbreaks with less psychological harm.”
— Public health psychologist involved in multiple outbreak responses

Where to Get Reliable, Up‑to‑Date Information
Because the situation can change, especially in the first days of an outbreak, always cross‑check the latest guidance from:
- World Health Organization – Nipah Virus Fact Sheet
- US Centers for Disease Control and Prevention – Nipah Virus (NiV)
- Ministry of Health and Family Welfare, Government of India
- National Centre for Disease Control (NCDC), India
Moving Forward: Calm, Informed Preparedness
The Nipah virus outbreak in West Bengal is serious, and it deserves attention—but not panic. While there is no specific cure or licensed vaccine yet, we are not helpless. Strong hygiene habits, safer caregiving, food precautions, and rapid public health action have successfully contained previous Nipah outbreaks in India and Bangladesh.
If you live in or near an affected area, your next steps are straightforward:
- Stay updated through official health channels, not rumors.
- Implement the practical safety measures outlined above at home and work.
- Seek medical care early if you or a loved one develops symptoms with relevant exposure.
- Support and check in on neighbors, especially the elderly or those living alone.
Prepared, informed communities are powerful. By focusing on what you can control, you help protect not just yourself but everyone around you.
