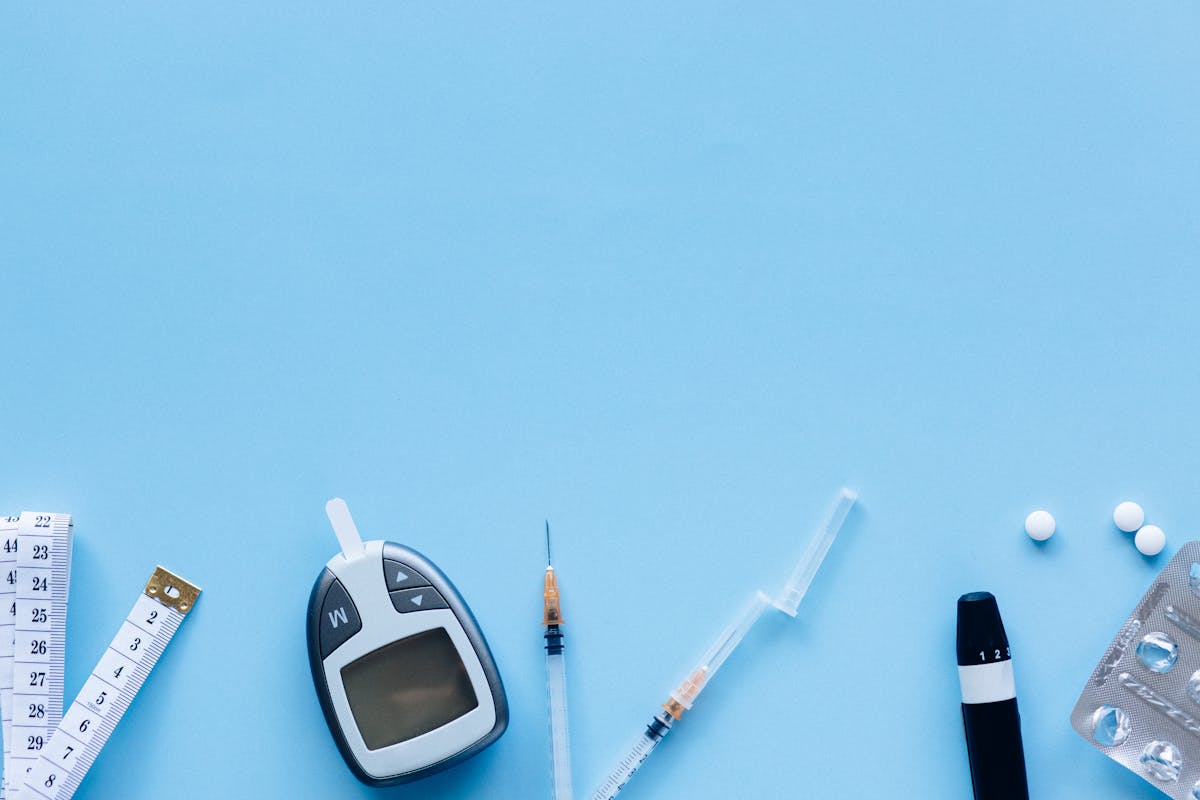
How Ozempic & Wegovy Are Changing Diet Culture (And What to Eat on GLP‑1s)
Ozempic, Wegovy & the GLP‑1 Weight‑Loss Diet Boom
GLP‑1 medications like Ozempic, Wegovy, Mounjaro, and Zepbound are changing the way we talk about weight loss, diet culture, and even everyday meals. Originally developed for type 2 diabetes, these drugs reduce appetite, slow digestion, and improve blood sugar control, often leading to significant weight loss. Alongside the excitement, there are important questions about nutrition, long‑term health, and how to eat well while taking them.
Below, we’ll explore why GLP‑1 drugs are trending, how they affect appetite and nutrition, what health professionals are recommending, and how to build balanced, satisfying meals that support your body—whether you’re on these medications or simply curious about this new era of weight‑loss science.
Why GLP‑1 Weight‑Loss Medications Are Trending Now
GLP‑1 receptor agonists have moved from quiet prescription pads into the spotlight of TikTok, Instagram, YouTube, and news headlines. They’ve become a cultural conversation about what it means to “diet” in 2026.
- Celebrity and influencer buzz: High‑profile users have turned medical treatments like Ozempic and Wegovy into lifestyle talking points, with dramatic before‑and‑after photos, red‑carpet speculation, and endless Q&A videos.
- Viral storytelling: Hashtags such as #ozempic, #wegovy, #mounjaro, and #ozempicweightloss host weekly weigh‑ins, side‑effect diaries, and “what I eat in a day on GLP‑1” clips that function as informal diet manuals.
- Shift in diet culture: Instead of centering only on willpower, macros, or trendy meal plans, conversations now frame obesity more as a chronic, treatable condition that can respond to medical therapy.
This visibility has brought genuine hope to many people who’ve struggled for years, while also raising concerns about misinformation, unrealistic expectations, and access for those who need these medications for diabetes or obesity management.
What Are GLP‑1 Medications and How Do They Affect Appetite?
GLP‑1 drugs like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) mimic or enhance the action of a hormone called glucagon‑like peptide‑1. In simple terms, they help your body:
- Feel full faster by acting on appetite centers in the brain.
- Slow gastric emptying, so food moves more slowly from your stomach to your intestines.
- Improve blood sugar control by boosting insulin release and reducing excess glucose production.
The lived experience many people describe is striking: what once triggered intense cravings—like sweets, fast food, or late‑night snacks—suddenly feels optional or even unappealing. Portion sizes shrink naturally. Restaurant meals stretch into two or three leftovers.
Nutritional Implications: Eating Well with Less Appetite
When appetite drops, diet quality matters more than ever. It becomes less about how much you eat and more about what you choose to put on that smaller plate.
- Risk: Too little protein. With tiny portions, it’s easy to fall short on protein, which can increase loss of muscle along with fat. Many dietitians suggest aiming for roughly 1.6–2.2 g of protein per kg of body weight per day for people actively losing weight, adjusted to individual needs and medical advice.
- Risk: Not enough fiber and micronutrients. When meals get smaller, fruits, vegetables, whole grains, nuts, and seeds may be crowded out by quick bites like crackers or coffee drinks.
- Opportunity: Better food choices. Many people naturally reduce intake of alcohol, ultra‑processed snacks, and sugary foods, which can improve blood pressure, blood sugar, and overall health.

A balanced GLP‑1‑friendly plate might feature a palm‑sized portion of lean protein, half a plate of colorful vegetables, and a small serving of whole grains or starchy vegetables, dressed with healthy fats for flavor and satisfaction.
“Ozempic Face,” Muscle Loss, and Body Composition
One widely discussed side effect of rapid weight loss is the so‑called “Ozempic face”—a gaunter appearance as fat and, potentially, some muscle are lost from the face and body. While some change in appearance is expected with significant weight loss, the pace and pattern can be unsettling.
Health professionals emphasize:
- Protecting lean mass: Combine higher‑protein eating with resistance training (like lifting weights or body‑weight exercises) to help preserve muscle.
- Avoiding extreme restriction: Very low calorie intake can accelerate loss of muscle and energy. Feel comfortably satisfied, not forced to eat nothing.
- Thinking long‑term: The goal is a healthier, stronger body composition, not just a lower number on the scale.
Changing Cravings and Your Relationship with Food
Many people on GLP‑1 medications describe a sense of freedom from cravings that once felt overpowering: sugary snacks, fast food, late‑night nibbling, or even alcohol lose their hold. This can be incredibly positive—but it can also create a new challenge: remembering to nourish yourself enough.
Some users report:
- Needing reminders or alarms to eat regular meals.
- A sudden disinterest in foods they used to love.
- Feeling guilty if they experience hunger at all, as if the medication should “fix” it.
A compassionate approach is key. Hunger is not a moral failing; it’s a normal, healthy signal. The goal with GLP‑1s is not to erase hunger completely, but to bring it into a manageable, less overwhelming range so you can make choices that feel peaceful and sustainable.
“The medication can quiet the noise around food, but you still deserve enough nourishment to feel strong, clear‑headed, and alive in your body.”
Debates, Ethics, and Access: Beyond the Hype
As GLP‑1 medications have gone mainstream, they’ve sparked serious debate about fairness, long‑term safety, and how they’re promoted online.
- Equity & access: In some regions, people with diabetes report difficulty accessing medications while celebrities or those with more resources use them for cosmetic weight loss. This raises questions about healthcare priorities and insurance coverage.
- Long‑term safety & weight regain: Early research is promising, but these drugs are still relatively new in widespread, long‑term use. Many people regain weight when stopping the medication if underlying habits and support systems haven’t changed.
- Ethical marketing: Social media clips may glamorize weight loss without clearly mentioning potential side effects like nausea, vomiting, diarrhea, constipation, or rarer complications such as gallbladder issues or pancreatitis.
Registered dietitians, physicians, and mental‑health professionals are increasingly stepping into the conversation with more balanced content: realistic expectations, side‑effect management, nutrition guidance, and reminders that body image is also an emotional journey, not just a medical one.
How to Eat on Ozempic, Wegovy & Other GLP‑1 Medications
While there’s no single “Ozempic diet,” nutrition professionals tend to agree on some guiding principles that support health, satisfaction, and sustainable weight management.
- Anchor meals around protein.
Include a high‑quality protein source at each meal: eggs, fish, poultry, lean meat, tofu, tempeh, lentils, beans, Greek yogurt, or cottage cheese. This helps protect muscle and steadies energy. - Fill half your plate with vegetables.
Think colorful: leafy greens, bell peppers, carrots, broccoli, cauliflower, tomatoes, cucumbers, squash. Fresh, frozen, and canned (low sodium) all count. - Add smart carbs for steady energy.
Whole grains (like oats, quinoa, brown rice), beans, lentils, and starchy vegetables (potatoes, sweet potatoes, corn) provide fiber and gentle, sustained energy. - Use healthy fats for flavor and satisfaction.
Olive oil, avocado, nuts, seeds, and fatty fish add richness that can make small meals feel indulgent rather than sparse. - Stay hydrated.
Sip water, herbal teas, or other low‑sugar beverages throughout the day. This supports digestion and can ease some GI side effects. - Listen to gentle hunger and fullness cues.
It’s okay to stop when you’re comfortably satisfied, even if your plate isn’t empty. It’s also okay to eat when you feel a mild, manageable hunger—your body still needs fuel.

A Sample “What I Eat in a Day” on GLP‑1 (Balanced Version)
Every body is different, and medical advice should be personalized. That said, here’s an example of how a gentle, nutrient‑dense GLP‑1 day of eating might look when appetite is lower than usual:
- Breakfast: Small bowl of Greek yogurt topped with berries, a spoonful of chia seeds, and a drizzle of honey; herbal tea or coffee with a splash of milk.
- Mid‑morning snack (if desired): Handful of roasted chickpeas or a small piece of cheese with a few whole‑grain crackers.
- Lunch: Half a whole‑grain wrap filled with grilled chicken or tofu, mixed greens, tomato, cucumber, and hummus; side of sliced bell peppers.
- Afternoon snack: A small apple with peanut butter, or a smoothie made with protein powder, frozen fruit, and spinach.
- Dinner: Baked salmon or lentil patties; roasted vegetables (like Brussels sprouts and carrots); a small serving of quinoa or brown rice with olive oil and lemon.
Portion sizes are intentionally modest, but every bite carries protein, fiber, and micronutrients to support your metabolism, muscles, and overall vitality.
Meal Prep, Storage, and Leftovers for Smaller Appetites
On GLP‑1 medications, it’s common to eat only part of a meal and save the rest. Thoughtful storage and reheating can turn those smaller portions into safe, delicious second (or third) meals.
- Safe storage: Refrigerate leftovers within 2 hours of cooking in shallow, airtight containers. Most cooked proteins, grains, and vegetables keep well for 3–4 days.
- Freezer‑friendly options: Soups, stews, cooked beans, chili, meatballs, and grain‑plus‑veggie mixes freeze beautifully in single‑serve containers, making it easy to grab a nourishing small meal anytime.
- Gentle reheating: Reheat in the microwave or on the stovetop until steaming hot (at least 74°C / 165°F). Add a splash of water or broth to prevent dryness, and finish with fresh herbs, lemon, or a drizzle of olive oil to brighten flavors.

Movement, Strength, and Life After GLP‑1 Medications
Exercise can feel more approachable when joints hurt less and breathing is easier, which often happens as weight decreases. Adding movement while on GLP‑1s pays dividends if you later reduce or stop the medication.
- Start gently: Even 10–15 minutes of walking after meals can support blood sugar control and digestion.
- Build strength: Two to three sessions per week of resistance training (weights, resistance bands, or body‑weight moves) help protect muscle and bone health.
- Think beyond the scale: Improved stamina, mood, sleep, and confidence are powerful markers of success, whether or not your weight stays at its lowest point.
For many, GLP‑1 medications are one chapter in a longer story. The habits you build around food, movement, sleep, and stress now can help soften weight regain and support metabolic health if your prescription or dosing changes down the road.
Key Takeaways: Navigating the GLP‑1 Weight‑Loss Era with Care
Ozempic, Wegovy, Mounjaro, Zepbound, and related GLP‑1 drugs have transformed the weight‑loss landscape and sparked new conversations about health, food, and fairness. Among all the noise, a few grounding truths stand out:
- These medications can be powerful tools for treating diabetes and obesity, but they’re not quick fixes or fashion accessories.
- Smaller appetites mean each bite matters—focus on protein, fiber, and nutrient‑dense foods.
- Preserving muscle and supporting mental health are just as important as the number on the scale.
- Long‑term success depends on sustainable habits, supportive healthcare, and realistic expectations about weight maintenance and regain.
If you’re considering or already using a GLP‑1 medication, working closely with your healthcare team—a doctor, registered dietitian, and, when possible, a mental‑health professional—can help you translate this powerful new tool into a healthier, more peaceful relationship with food and your body.

