How a Common “Kissing Disease” May Shape Your Risk for Autoimmune Illness
Scientists have inched closer to solving the mystery of the “kissing disease,” or mononucleosis, by identifying 22 genes that appear to raise the risk of autoimmune conditions such as lupus, rheumatoid arthritis, and even stroke in people infected with the Epstein–Barr virus (EBV). In plain language, this research helps explain why a virus that most of us catch at some point in life may become a long‑term health problem for a small minority.
If you’ve ever had mono—or know someone who has—it’s normal to feel uneasy reading headlines that link it to serious disease. Let’s walk through what scientists have actually found, what it does (and doesn’t) mean for your health, and what practical steps you can take without panic.
The “Kissing Disease” Mystery: Why Scientists Care So Much About Epstein–Barr Virus
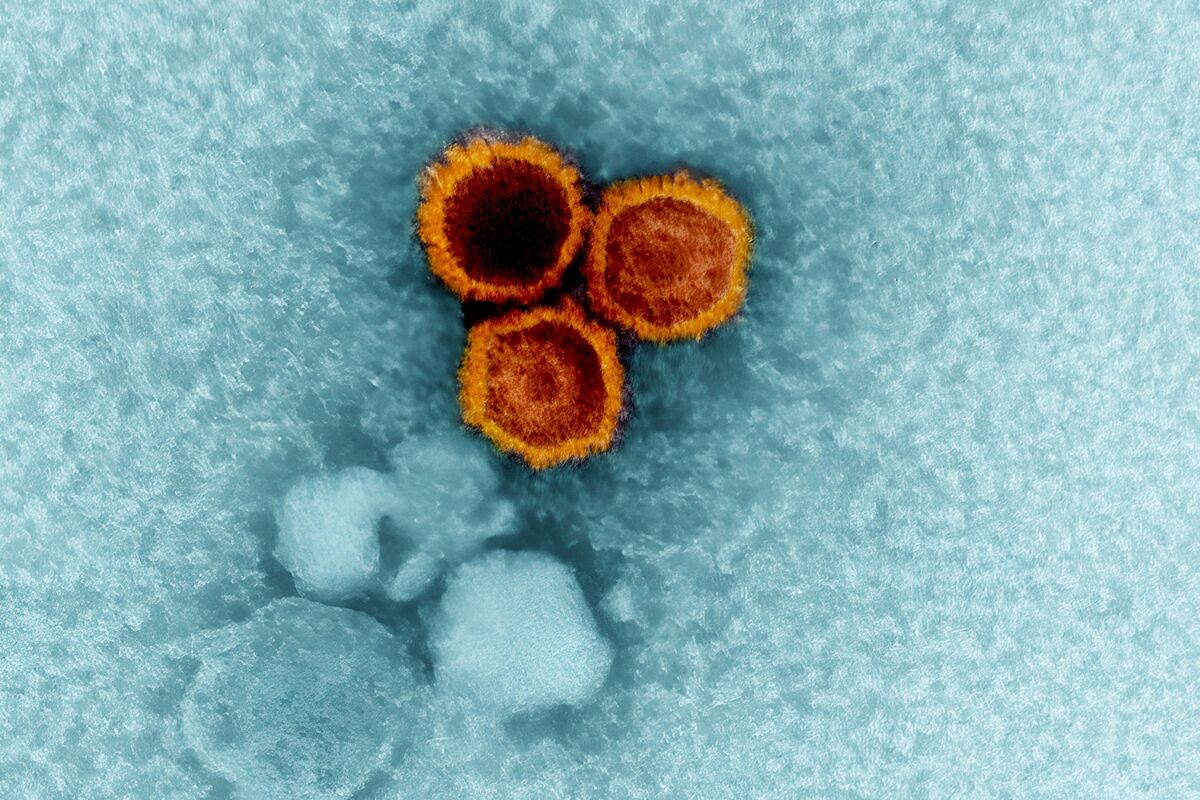
Epstein–Barr virus is incredibly common—over 90% of adults worldwide carry it. It’s often spread through saliva, which is why mono picked up the nickname “kissing disease,” though it’s also passed by sharing drinks, utensils, or close contact.
For most people, EBV infection:
- Happens in childhood or adolescence
- Causes mild symptoms—or none at all
- Leads to lifelong, usually quiet, infection in immune cells
A small percentage, however, develop classic mononucleosis symptoms:
- Extreme fatigue
- Sore throat and swollen glands
- Fever and body aches
- Occasionally enlarged liver or spleen
For decades, researchers have noticed that people with certain autoimmune diseases are more likely to have signs of past EBV infection. What hasn’t been clear is why that happens—or who is actually at risk.
“EBV is like a spark. Whether it fizzles out or lights a fire may depend heavily on your genes and your immune system’s timing.”
— Immunology researcher, summarized from recent literature
What the New Study Found: 22 Genes That May Link Mono to Autoimmune Disease
According to recent reporting from Bloomberg and related scientific publications, scientists have identified 22 genes that seem to increase the risk of conditions like:
- Systemic lupus erythematosus (lupus)
- Rheumatoid arthritis
- Certain types of stroke
- Other autoimmune and inflammatory disorders
These genes are involved in how your immune system responds to EBV. Researchers used advanced tools—like genome-wide association studies and analyses of how viral proteins interact with human DNA—to pinpoint which genetic regions might make EBV infection more likely to trigger long‑term immune problems.
Think of these genes as making your immune system’s “volume knob” a bit more sensitive. When EBV shows up, the response in some people may be overly strong or misdirected, increasing the chance that the immune system accidentally attacks the body’s own tissues.

Should You Be Worried If You’ve Had Mono?
It’s understandable to feel anxious if you had mono in high school or college and are now hearing about genetic links to serious diseases. Here’s the balanced view based on current evidence:
- EBV infection is nearly universal. Most adults have it, but only a minority develop autoimmune disease.
- Genes are only part of the story. Environment, hormones, lifestyle, and chance also play major roles.
- Risk is relative, not absolute. A “higher” risk might still be low in real‑world numbers for any individual.
In clinic, many people share a similar worry:
“I had a terrible case of mono in college. Now that I’m hearing about lupus and stroke, I’m scared something is brewing inside me.”
When doctors evaluate someone like this, they don’t jump straight to worst‑case scenarios. Instead, they look at:
- Current symptoms (joint pain, prolonged fatigue, rashes, unexplained fevers)
- Family history of autoimmune disease or early stroke
- Other risk factors (smoking, blood pressure, cholesterol, infections)
How a Virus and Your Genes Might Team Up: The Science in Simple Terms
Researchers are piecing together how EBV might contribute to autoimmune disease in some genetically susceptible people. While details continue to evolve, a few mechanisms keep showing up in the scientific literature:
- Molecular mimicry: Some EBV proteins may resemble human proteins, confusing the immune system so it attacks both.
- Chronic immune activation: EBV can linger quietly in B cells, occasionally reactivating and nudging the immune system over and over.
- Direct interference with DNA regulation: Viral proteins can bind to human DNA or regulatory regions, subtly changing how immune‑related genes turn on and off.
The newly identified 22 genes appear to sit at crossroads of these pathways, influencing how strongly and in what direction your immune system reacts to EBV.

Practical Steps You Can Take If You’ve Had Mono or EBV
While you can’t change your genes or “erase” EBV, you can influence how your immune system and blood vessels behave over time. The same habits that support general health also seem to lower the risk of many autoimmune and cardiovascular problems.
1. Stay on top of routine check‑ups
- Check blood pressure, cholesterol, blood sugar, and weight regularly.
- Share your history of severe mono with your clinician, especially if you develop new, unexplained symptoms.
- Ask about personalized screening if you have a strong family history of autoimmune disease.
2. Support your immune system (without extreme “hacks”)
- Prioritize 7–9 hours of sleep per night.
- Choose a mostly plant‑forward, minimally processed diet (e.g., Mediterranean‑style eating).
- Engage in regular movement—aim for at least 150 minutes per week of moderate activity, if medically safe.
- Avoid smoking and limit alcohol intake.
3. Watch for early warning signs
Seek medical advice if you notice:
- New joint pain, swelling, or morning stiffness lasting weeks
- Persistent, unexplained fatigue
- Frequent mouth ulcers or rashes, especially with sun exposure
- Shortness of breath, chest pain, or neurologic symptoms (sudden weakness, trouble speaking, or vision changes—these are emergencies)
Common Obstacles: Anxiety, Misinformation, and “Miracle Cure” Promises
New science often brings a wave of confusing and sometimes scary headlines. When it comes to EBV, several challenges tend to show up:
- Anxiety: Learning that a common virus is linked to serious illness can feel overwhelming.
- Misinformation: Social media may exaggerate risks or promote unproven “EBV detox” protocols.
- All‑or‑nothing thinking: People may assume that because a risk exists, disease is inevitable.
“I went down an internet rabbit hole and came out convinced EBV was the cause of every symptom I’d ever had.”
— Patient anecdote, paraphrased from clinic experience
Here are some ways to protect yourself:
- Rely on reputable sources (major medical centers, peer‑reviewed journals, established news outlets that cite experts).
- Be skeptical of anyone selling high‑priced supplements or “cures” specifically for EBV without solid clinical trials.
- Use your anxiety as a cue to schedule a check‑in with your clinician rather than self‑diagnosing online.
What This Could Mean for the Future: Vaccines and Targeted Therapies
One of the most hopeful aspects of this research is that it may lay the groundwork for prevention and precision medicine.
- EBV vaccines: Several groups, including large pharmaceutical companies and academic centers, are exploring EBV vaccine candidates. The goal would be to prevent mono and possibly lower downstream autoimmune and cancer risks, though this is still under active study.
- Risk‑based monitoring: In the future, knowing which genes interact with EBV could help identify people who might benefit from closer follow‑up after infection.
- Targeted drugs: Understanding how EBV proteins affect immune pathways may point to new drug targets for autoimmune diseases.
These are long‑term prospects, not tomorrow’s treatments, but they underscore why this genetic research matters on a global scale.

Bringing It All Together: Informed, Not Alarmed
Scientists are steadily untangling how a very common virus, Epstein–Barr, might contribute to serious but relatively uncommon diseases in genetically susceptible people. Identifying 22 risk‑related genes is a meaningful step forward in solving the “kissing disease” mystery, but it does not mean that everyone who’s had mono is destined for lupus, arthritis, or stroke.
Your most powerful tools remain:
- Consistent, preventive health care
- Everyday habits that support immune and cardiovascular health
- Staying curious and informed, while avoiding panic and hype
If this topic hits close to home—perhaps because you had severe mono, live with ongoing fatigue, or have a family history of autoimmune disease—consider using what you’ve learned here as a starting point for a thoughtful, honest conversation with your health‑care team.
You don’t need to fear your past infection, but you can let this new science motivate you to be an active partner in your long‑term health.
Learn More: Trusted Resources on EBV and Autoimmune Disease
For readers who want to dive deeper into the science and clinical guidance, these reputable organizations and publications provide regularly updated information:
- U.S. Centers for Disease Control and Prevention (CDC) – Epstein–Barr Virus
- National Institute of Allergy and Infectious Diseases (NIAID) – EBV Information
- Lupus Foundation of America – EBV and Lupus Overview
- Arthritis Foundation – Rheumatoid Arthritis
- American Heart Association – Stroke Journal (for research‑minded readers)
As new research on EBV and these 22 genes emerges, these sources are likely to highlight major developments and potential changes in clinical recommendations.
