Could a Single Injection Help Your Knees Grow New Cartilage? Inside the Breakthrough That Might Delay Knee Replacements
Anti-Aging Knee Injection: What the New Cartilage Regrowth Breakthrough Really Means for You
If you live with knee pain—whether from an old sports injury, years of wear and tear, or early arthritis—you’ve probably wondered if there’s anything that can actually restore your joints, not just numb the pain. A new study making headlines suggests an anti-aging drug may help regrow knee cartilage and prevent arthritis, at least in mice, raising big questions about the future of knee replacements.
In this guide, we’ll break down what researchers really found, how this potential treatment works, and what it could one day mean for people facing knee surgery—without overhyping early results. We’ll also cover evidence-based steps you can take right now to protect your knee cartilage while science catches up.
The Problem: Why Knee Cartilage Loss Leads to Pain and Replacements
Your knee is a complex hinge joint where the thigh bone (femur), shin bone (tibia), and kneecap (patella) meet. The smooth, rubbery tissue covering the ends of these bones—articular cartilage—acts like a cushion and gliding surface.
The challenge is that cartilage has very limited ability to heal. Once it wears down or is damaged:
- Joint surfaces become rough, leading to friction and stiffness.
- Inflammation increases, contributing to osteoarthritis.
- Pain and loss of function can make everyday tasks—like climbing stairs—difficult.
For many people, the final step is a total knee replacement, a major surgery in which damaged joint surfaces are replaced with artificial components. While often effective, it comes with:
- Significant recovery time and rehab.
- Risks of complications, especially with other health conditions.
- A limited lifespan of the prosthetic joint, which can be an issue for younger patients.
“For decades, we’ve gotten better at replacing knees, but not at truly restoring the original cartilage. Any therapy that can safely regrow or preserve cartilage would be a game-changer—if it works in humans.”
— Hypothetical comment, Dr. A. Patel, orthopedic surgeon
The Breakthrough: An Anti-Aging Drug That Regrows Knee Cartilage in Mice
According to a January 2026 report in Good News Network, researchers have developed an injection that blocks a specific biological pathway linked to aging. In animal studies, this treatment:
- Regrew cartilage in the knees of aged mice.
- Prevented the development of arthritis after knee injuries such as ACL tears in mice—injuries that commonly trigger arthritis in humans.
- Made the cartilage in older, treated mice resemble that of much younger mice under the microscope.
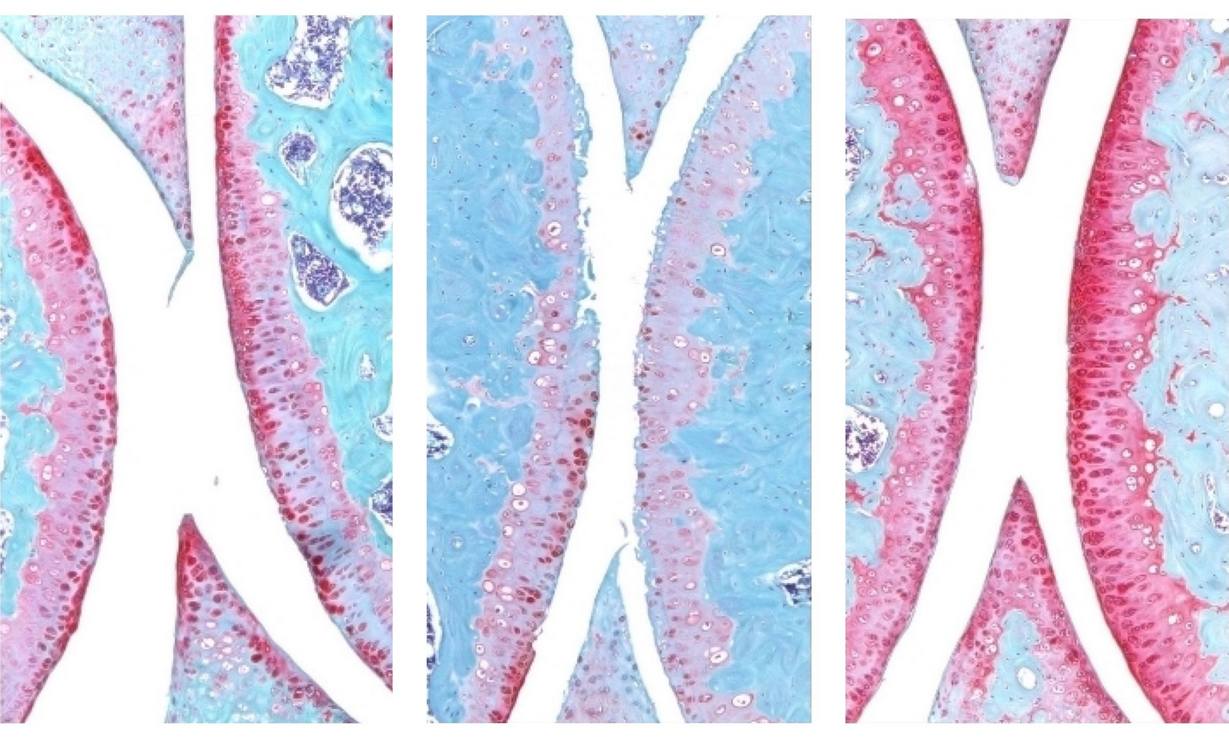
Images shared by the research team show clear differences in cartilage thickness and coverage between:
- Young healthy mouse knees (robust red-stained cartilage).
- Older mouse knees (thinned, degraded cartilage).
- Older mice treated with the drug (restored, more youthful-looking cartilage).
Although popular coverage refers to this as an “anti-aging drug,” it’s more accurate to say that the injection targets molecular pathways involved in age-related cartilage breakdown and post-injury degeneration. By interrupting those signals, cells in the joint environment may behave more like they do in youth—producing and maintaining healthy cartilage.
How the Anti-Aging Knee Injection Likely Works (In Plain English)
While the specific drug and pathway are still being studied, this approach falls into a broader category of senescence and inflammation-targeting therapies. In aging joints:
- Cells can become “senescent”—alive but dysfunctional, secreting inflammatory chemicals.
- These chemicals accelerate tissue breakdown, including cartilage loss.
- Injury (like an ACL tear) can amplify this inflammatory environment.
The studied injection appears to:
- Block harmful signaling linked to aging and inflammation in the joint.
- Reduce destructive activity that normally wears down cartilage.
- Support cartilage-producing cells so they can rebuild and maintain healthy tissue.
This fits into a wider movement in medicine that focuses not only on treating symptoms (like pain), but modifying the underlying disease process—in this case, osteoarthritis and post-traumatic arthritis.
Could This End Knee Replacements? A Realistic Look
Headlines suggesting this breakthrough could “end knee replacements” are understandably exciting, but the science isn’t there yet. Here’s a realistic breakdown:
- Mouse success ≠ human guarantee. Many therapies that work in animals don’t fully translate to people.
- Complex knees, complex lives. Human knees endure decades of load, past injuries, weight changes, and other health conditions that mice never face.
- Dosing and safety need careful testing. A drug that helps cartilage might affect other tissues or systems.
Where experts are cautiously optimistic is in the idea that, if similar results appear in human clinical trials, this type of therapy might:
- Delay the need for knee replacements in some patients.
- Protect knees after injury, reducing the chance of developing arthritis later.
- Improve quality of life by preserving more of a person’s natural joint function.
“I tell patients that breakthroughs like this give us hope for the next decade, not the next doctor’s appointment. Right now, our best tools are still exercise, weight management, joint-friendly activities, and when necessary, surgery.”
— Hypothetical comment, Dr. L. Nguyen, sports medicine physician
How Close Are We? Likely Timeline from Lab to Clinic
As of early 2026, the anti-aging cartilage-regrowing injection is still in the preclinical / early research stage. A typical path to patient use includes:
- Preclinical studies in animals (already underway).
- Phase I trials in small groups of healthy volunteers or patients to assess safety and dosing.
- Phase II trials to see whether it helps the target condition and refine dosage.
- Phase III trials in larger, diverse patient groups to confirm effectiveness and monitor side effects.
- Regulatory review (e.g., FDA, EMA) and then gradual clinical rollout, if approved.
Even for promising treatments, this process typically takes years, not months. Timelines can shorten with strong results and streamlined pathways, but any claims that this injection will “end knee replacements soon” are speculative.
What You Can Do Now: Proven Ways to Protect and Support Your Knees
While we wait for regenerative injections to mature, there is strong evidence for several practical, accessible strategies that can significantly reduce knee pain and slow cartilage wear.
1. Build Strong, Supportive Muscles
Research consistently shows that strengthening the quadriceps, hamstrings, glutes, and calf muscles reduces knee pain and improves function in osteoarthritis.
- Start with low-load exercises like sit-to-stands, step-ups, mini-squats, and bridges.
- Use resistance bands or light weights as tolerated.
- Work with a physical therapist if pain or fear of movement is a barrier.
2. Keep Moving, But Smartly
Complete rest can weaken muscles and stiffen joints. Instead, focus on low-impact, joint-friendly activities:
- Walking on level ground.
- Cycling or stationary biking.
- Swimming or water aerobics.
- Elliptical training.
3. Manage Body Weight When Possible
Extra body weight increases the load on your knees with every step. Studies show that modest weight loss (5–10% of body weight) can meaningfully reduce knee pain and improve function in people with osteoarthritis.
4. Supportive Footwear and Surfaces
Wearing cushioned, supportive shoes and walking on softer surfaces (grass, tracks) can reduce joint stress compared with hard concrete in unsupportive footwear.
5. Evidence-Based Medical Care
Work with your healthcare provider to tailor a plan that may include:
- Physical therapy (often one of the most impactful tools).
- Medications like NSAIDs, if appropriate, to manage flare-ups.
- Injections such as corticosteroids or hyaluronic acid—these do not regrow cartilage, but can provide symptom relief for some.
- Surgical options when conservative care is no longer enough.

Preventing Post-Injury Arthritis: Lessons from the ACL Mouse Study
A key part of the new research is that the injection helped prevent arthritis after ACL-like injuries in mice. In humans, ACL tears and meniscus injuries are known to sharply increase the risk of early osteoarthritis, even when surgery is performed.
While you can’t yet get an “arthritis-preventing injection” after injury, you can:
- Rehab thoroughly after injuries and surgeries—don’t rush back before strength, balance, and control are restored.
- Protect your knees in high-risk sports (proper footwear, training, and technique).
- Address alignment or muscle imbalances that could overload certain parts of the knee.
A Real-World Story: Combining Hope for the Future with Action Today
A patient I’ll call “Mark,” a 52-year-old recreational basketball player, came into clinic after years of on-and-off knee pain from an old meniscus tear. He’d seen a headline about “anti-aging injections that regrow cartilage” and asked if he could get it instead of considering surgery.
We talked through the current science—promising mouse data, but no approved human treatment yet—and focused on what he could control:
- A structured strength program focused on quads, hips, and core.
- Switching some high-impact court time to cycling and swimming.
- Losing about 15 pounds over six months, with help from a dietitian.
Six months later, Mark’s knee pain wasn’t “cured,” but he reported he could play half-court games without limping the next day and no longer dreaded stairs. He still follows news about new treatments—and he may one day be a candidate for regenerative therapies—but he’s not waiting passively for a future injection to save his knees.
What the Science Says: Arthritis, Cartilage, and Regeneration
While the full details of the new anti-aging drug study are still emerging, it fits into a broader landscape of arthritis research:
- Disease-modifying osteoarthritis drugs (DMOADs) are being studied to slow or reverse joint damage, but none are fully established in routine clinical practice yet.
- Senolytic therapies (drugs that target senescent cells) have shown cartilage-protective effects in some animal models.
- Biologic agents that block inflammatory cytokines are used in inflammatory arthritis (like rheumatoid arthritis), though osteoarthritis is more complex and mechanical.
For reliable, up-to-date information on emerging treatments and knee osteoarthritis, consider resources like:
Before and After: Lab Images vs. Real-Life Expectations
The mouse images from the study are compelling: thin, patchy cartilage in aged knees compared with thicker, more complete coverage after treatment. They suggest that, at least in a controlled lab setting, it’s possible to restore cartilage-like tissue where it had been lost.

In real life, your experience will depend on factors such as:
- How advanced your arthritis is.
- Your overall health, activity level, and body weight.
- Previous injuries or surgeries.
- How consistently you follow a strengthening and activity plan.
Even if future injections can regrow cartilage in humans, they will most likely be part of a comprehensive approach that still includes movement, strength, and lifestyle adjustments—not a one-time magic fix.
Moving Forward: Hope Without Hype for Healthier Knees
The news that an anti-aging drug can regrow knee cartilage and prevent arthritis in mice is genuinely encouraging. It signals a future where, instead of waiting for joints to fail and replacing them, we may be able to protect and restore them earlier.
At the same time, staying grounded is essential. As of 2026, these injections are not available for routine clinical use, and we don’t yet know how well they’ll perform in human knees. What we do know is that your daily choices still matter enormously for pain, mobility, and long-term joint health.
If you’re dealing with knee pain today, consider this a two-track plan:
- Act now: Work with a healthcare professional or physical therapist to build strength, adjust activities, manage weight where possible, and explore current evidence-based treatments.
- Stay informed: Keep an eye on reputable sources for updates on regenerative therapies, and be cautious of unproven “miracle” injections marketed ahead of the science.
You don’t have to choose between hope for the future and action today. You can do both—caring for the knees you have now, while science works toward even better options in the years ahead.

