New Breakthrough to Strengthen Bones: Can We Finally Turn the Tide on Osteoporosis?
Updated: December 2, 2025
A New Hope for Fragile Bones: What This Osteoporosis Breakthrough Really Means
If you’ve ever watched a parent or grandparent struggle after a hip or spine fracture, you know how life-changing osteoporosis can be. The fear of “one bad fall” is real—and it can quietly shape the way you move, travel, or even play with your kids or grandkids.
A new study reported by ScienceAlert highlights a powerful bone-strengthening mechanism inside the body that scientists are now learning how to target. Early findings suggest that, one day, we may be able not just to slow osteoporosis, but potentially help reverse some of the bone loss that makes fractures so likely.
In this guide, we’ll walk through what researchers have found, what it realistically means for people living with osteoporosis today, and the evidence-based steps you can take right now to support stronger bones—without hype or false promises.
Why Osteoporosis Is Such a Tough Problem
Osteoporosis is often called a “silent disease” because bone loss happens gradually and without pain—until a fracture occurs. By then, bone density may have declined for years or even decades.
Globally, hundreds of millions of people are affected, especially:
- Postmenopausal women
- Adults over 65 of any sex
- People with long-term steroid use, certain autoimmune or digestive diseases
- Those with a family history of osteoporosis or hip fracture
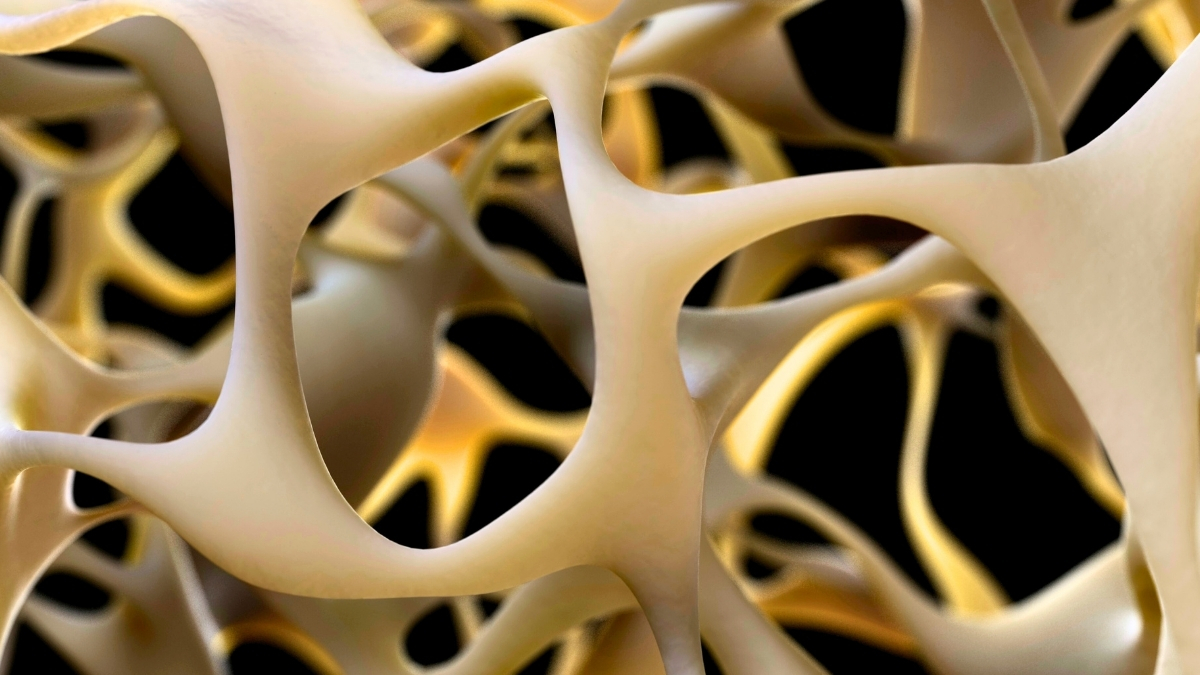
The challenge: our bones are constantly being remodeled. Specialized cells called osteoclasts break down old bone, while osteoblasts build new bone. With age, hormonal shifts, inactivity, or illness, that balance tilts toward breakdown. Traditional osteoporosis treatments either slow down bone breakdown, boost bone formation, or both—but none are perfect, and some people still fracture despite treatment.
Inside the New Bone-Strengthening Breakthrough
The new research, led by scientists at the University of (as reported by ScienceAlert), zeroes in on a specific biological pathway that helps bones sense and respond to mechanical stress—things like walking, lifting, or even everyday movement.
While the exact molecules and gene targets are still being mapped, the core idea is this:
- Bone cells detect mechanical strain (for example, from weight-bearing exercise).
- This triggers a signaling cascade inside the bone.
- Certain proteins switch on genes that favor bone formation and strengthen bone microstructure.
In lab and early animal models, researchers were able to:
- Amplify this bone-strengthening signal
- Reduce the usual age-related or hormone-related bone loss
- Improve bone quality—not just quantity—by enhancing internal architecture
“We’re not just adding more bone; we’re nudging the body to build better-quality bone in the right places,” one of the study’s senior authors explained in the ScienceAlert report.
That distinction matters. Bone density numbers on a scan (like a DEXA) are important, but the way bone is organized inside—the tiny struts and networks that make it strong—may be just as critical for preventing fractures.
Can Osteoporosis Really Be Reversed?
It’s natural to hear “reverse osteoporosis” and feel hopeful—or skeptical. The truth, based on current evidence, sits somewhere in the middle.
Today’s strongest osteoporosis medications (such as anabolic agents like teriparatide or romosozumab, along with antiresorptive drugs like bisphosphonates) can:
- Increase bone mineral density (BMD) at the spine and hip
- Reduce the risk of certain fractures
- Partially restore bone microstructure in some people
But they usually don’t “reset” bone completely to its youthful state—especially after decades of bone loss or multiple fractures. The emerging bone-strengthening pathway highlighted in the new study could, in theory, push us closer to:
- More targeted bone building, where it’s needed most (like the hip and spine)
- Better quality bone, not just higher BMD scores
- Combination treatments that both stop breakdown and optimize new bone formation
Still, no current or near-term therapy can guarantee that osteoporosis will be fully reversed or that fractures will never happen. What we can say, supported by multiple clinical trials, is that:
- The right medications do substantially lower fracture risk for many people.
- Even modest gains in bone density can have meaningful benefits.
- Lifestyle changes can complement, but not replace, medical treatment when osteoporosis is significant.
What You Can Do Right Now to Strengthen Your Bones
While we wait for new therapies based on this discovery to move through clinical trials, there is a lot you can do today to support bone health. These aren’t quick fixes—but they are backed by decades of research.
1. Prioritize Bone-Active Nutrition
Think of food as the raw material your new bone cells need to build with.
- Calcium: Aim for about 1,000–1,200 mg/day from food and supplements combined (check with your clinician for your exact target). Good sources:
- Low-fat dairy, yogurt, cheese
- Calcium-fortified plant milks and juices
- Leafy greens like kale and bok choy
- Canned salmon or sardines with bones
- Vitamin D: Helps your body absorb calcium. Many adults need 800–1,000 IU/day, sometimes more if levels are low, but blood testing is the safest guide.
- Protein: Adequate protein supports both muscle and bone. Most adults do well with ~1.0–1.2 g/kg body weight per day, unless your doctor advises otherwise.
- Other nutrients: Magnesium, vitamin K, and trace minerals also play supporting roles in bone metabolism.

2. Use Movement to “Speak” to Your Bones
The same mechanical signals the new study is trying to harness pharmaceutically are also triggered—naturally—by the way you move.
- Weight-bearing exercise: Walking, stair climbing, dancing, low-impact aerobics. Aim for:
- 150–300 minutes per week of moderate-intensity activity, as tolerated.
- Resistance training: Bands, free weights, or machines 2–3 times per week can stimulate both muscle and bone.
- Balance and posture work: Tai chi, yoga (with modifications if you have vertebral fractures), or targeted physical therapy can reduce fall risk.
Always ask your provider or a physical therapist which movements are safe for your spine and hips, especially if you already have osteoporosis or past fractures.
3. Minimize Bone “Saboteurs”
Some everyday habits quietly tip the balance toward bone loss.
- Smoking: Linked to lower bone density and higher fracture risk.
- Excess alcohol: More than 1 drink per day (women) or 2 (men) is associated with weaker bones.
- Very low-calorie or restrictive diets: Can deprive bones of critical nutrients and hormones.
- Prolonged immobility: Long periods in bed or sitting accelerate bone breakdown.
Real-World Obstacles—and How People Overcome Them
Knowing what to do is one thing. Living with osteoporosis—pain, fear of falling, fatigue, or other conditions at the same time—can make it tough to follow through.
“I’m Scared to Move—What If I Break Something?”
This fear is incredibly common, especially after a first fracture. Ironically, avoiding movement can weaken muscles and bones further, increasing future risk.
In clinic, many patients do better when:
- They start with supervised physical therapy focused on safe, gentle movements.
- They practice getting up from chairs, walking short distances, and improving balance before progressing.
- They receive clear written guidance on which motions to avoid (for example, deep spine flexion) and which are encouraged.
“Medications Worry Me—Are They Worth It?”
Concerns about side effects are valid. While rare complications from osteoporosis drugs do exist, the risk of serious fracture—especially hip fracture—often outweighs these risks for people with low bone density and previous fractures.
A helpful framework:
- Ask your clinician about your absolute fracture risk over the next 10 years.
- Discuss the benefits and side effects of each medication option with real numbers, not just general warnings.
- Revisit the decision periodically; you’re not locked into one path forever.
“When patients understand their actual fracture risk and how a medication changes that risk, decisions feel less scary and more collaborative,” notes a metabolic bone specialist interviewed in similar research summaries.
How This Discovery Fits into the Bigger Osteoporosis Research Picture
The newly identified bone-strengthening mechanism builds on several existing scientific themes:
- Mechanotransduction: The process by which cells convert physical forces into biochemical signals. This is a hot area in bone research, especially involving osteocytes (the “sensor” cells embedded in bone).
- Wnt signaling and related pathways: Known to be crucial in bone formation; some current osteoporosis drugs already act on these signals.
- Combination therapies: Researchers are increasingly exploring sequences or combinations of bone-building and bone-preserving drugs for maximal effect.
Early-stage findings like this often take years to translate into approved treatments. Steps typically include:
- Confirming the mechanism in multiple animal models.
- Testing safety and dosing in small human Phase I trials.
- Evaluating effectiveness in larger Phase II and III trials.
- Ongoing monitoring after approval to track real-world outcomes and rare side effects.

From Fragile to Stronger: A Realistic “Before and After”
When we talk about “reversing osteoporosis,” it helps to set realistic expectations about what meaningful improvement can look like in everyday life.


In many case reports and clinical experiences, the most powerful “after” isn’t a perfect scan—it’s:
- Fewer or no new fractures over several years
- Improved balance and strength
- Returning to valued activities with more confidence
- Feeling informed and in control of your choices
Turning New Science into Personal Action
This new bone-strengthening breakthrough is genuinely exciting. It deepens our understanding of how bones respond to stress and opens doors to future therapies that may better repair or even partly reverse osteoporosis-related damage.
At the same time, your bones can’t wait for the perfect pill. The choices you and your care team make over the next 6–12 months—about movement, nutrition, medications, and fall prevention—can meaningfully change your fracture risk, regardless of age.
Three steps you can take this week:
- Ask your clinician whether you need a DEXA scan or an update on your current bone density results.
- Start or refine a safe, bone-friendly activity plan (even 10-minute walks are a great start).
- Audit your daily calcium, vitamin D, and protein intake, and adjust with food or supplements as advised.
New science is expanding what’s possible for treating osteoporosis. Your daily actions—and an informed partnership with your healthcare team—remain the most powerful tools you have right now to protect and strengthen your bones.
