Can Two Common Supplements Really Help Fight Deadly Brain Cancer? What the New Glioblastoma Research Reveals
Hearing the word “glioblastoma” in a doctor’s office can feel like the floor has dropped away. It’s one of the most aggressive brain cancers we know, and current treatments, while vital, are often limited in how long they can keep the disease at bay. So when headlines announce that a “simple supplement combo” might help fight glioblastoma, it’s natural to feel a surge of hope—and a lot of questions.
A recent study, reported by ScienceAlert, has explored the use of two widely available supplements on glioblastoma tumor cells. The early findings are encouraging, but they are also preliminary. In this article, we’ll unpack what the research actually shows, how these supplements might work, where the science stands today, and what patients and families should carefully consider before making any changes.
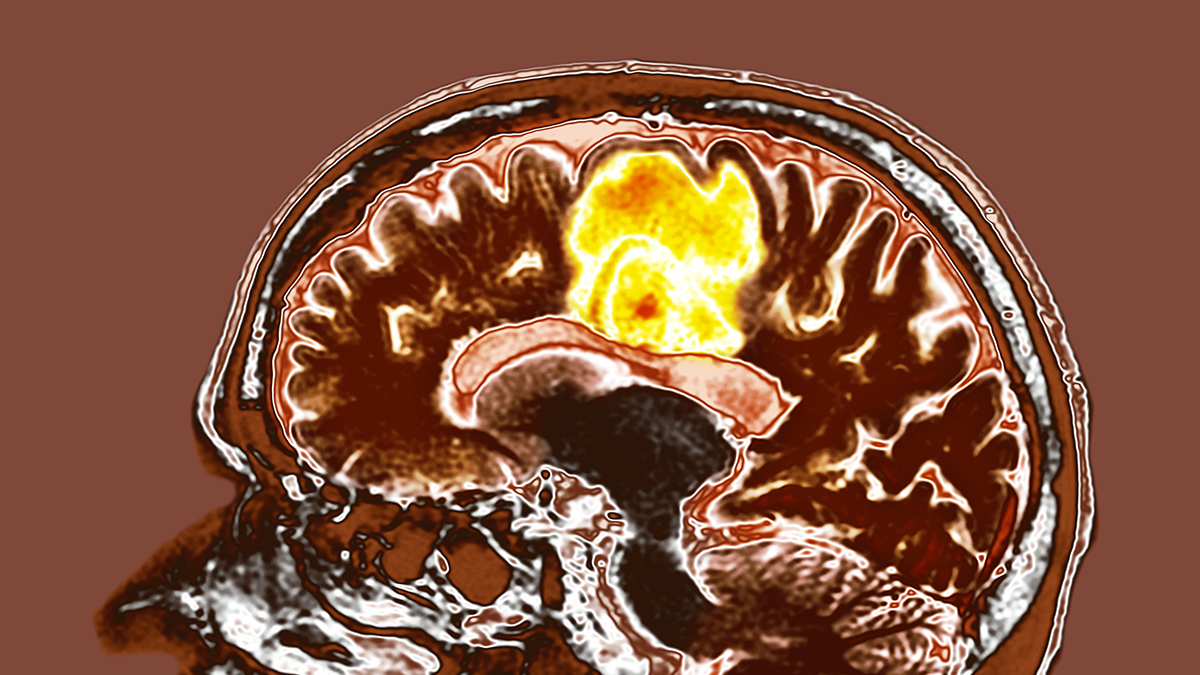
Understanding Glioblastoma: Why It’s So Hard to Treat
Glioblastoma (often called GBM) is a fast-growing brain cancer that tends to invade nearby brain tissue, making it very difficult to remove completely with surgery. Standard care usually includes:
- Surgery to remove as much of the tumor as safely possible
- Radiation therapy to target remaining cancer cells
- Chemotherapy, most often with temozolomide
Even with aggressive treatment, glioblastoma often returns. One reason is that GBM cells are remarkably adaptable: they can shift their metabolism (how they use energy and nutrients) and resist many forms of stress, including drugs and radiation.
“Glioblastoma is not just one disease—it’s a whole ecosystem of cancer cells that can change their behavior to survive. Targeting their metabolism is an emerging strategy we’re watching closely.”
— Neuro-oncologist, academic medical center (commenting on current research trends)
This metabolic flexibility is exactly what some new studies, including the supplement-combination research, are trying to exploit.
The “Simple Supplement Combo” Study: What Did Researchers Actually Test?
The ScienceAlert report describes research in which scientists tested a combination of two common supplements on glioblastoma tumor models. While media summaries can be brief, the core idea is:
- The supplements were chosen because they influence how cells handle energy and stress.
- Researchers applied them to glioblastoma cells or tumor samples in controlled lab conditions.
- They measured changes such as tumor cell growth, survival, and metabolic markers.
In plain language, the goal was to see whether tweaking the tumor’s metabolism using substances already available to the public might make the cancer weaker or more sensitive to treatment.
How Might a Supplement Combination Weaken Glioblastoma?
While specific details depend on the exact compounds studied, many of the supplement strategies being explored in glioblastoma focus on the same broad targets:
- Tumor metabolism: GBM cells often rely heavily on certain fuel sources (like glucose) and pathways. Some supplements may push these cells into “energy stress,” where they struggle to grow.
- Oxidative stress: Cancer cells live with a delicate balance of reactive oxygen species. Pushing that balance too far can damage or kill them—but it can also harm healthy cells if not carefully controlled.
- Cell signaling pathways: Nutrient-sensing pathways (such as AMPK or mTOR) help cells decide whether to grow, divide, or conserve resources. Some supplements can nudge these pathways toward slowing growth.
Different combinations aim to “hit” several of these weak spots at once, hoping to make glioblastoma cells less resilient, more sensitive to standard treatments, or slower to regrow.

“Targeting cancer metabolism with non-toxic agents, including some supplements, is a promising area of research. But dosing, timing, and interactions with standard therapy need careful testing in clinical trials.”
— Translational cancer researcher, metabolic oncology group
What the Evidence Shows So Far (And What It Doesn’t)
Based on current reports, including the work highlighted by ScienceAlert, here’s what we can reasonably say:
- Some supplement combinations can alter glioblastoma cell behavior in lab settings.
- In experimental models, certain combos may slow tumor growth or increase signs of cell stress or death.
- These findings support the idea that glioblastoma’s metabolism is a valid therapeutic target.
However, we cannot yet say:
- That these supplements improve survival in people with glioblastoma.
- What the safest and most effective dose or schedule would be in humans.
- How they interact with chemotherapy, radiation, steroids, or seizure medications.
For up-to-date, peer-reviewed information, it’s worth searching clinical trial registries (for example, ClinicalTrials.gov) for “glioblastoma” and “metabolism,” “dietary supplement,” or specific compound names once they’re publicly identified.
Safety First: Why “Common” Supplements Can Still Be Risky in Brain Cancer
It’s tempting to think, “If I can buy it at the store, it must be safe.” But in the setting of glioblastoma—and the powerful treatments that accompany it—supplements can have real risks:
- Drug interactions: Some supplements affect liver enzymes that process chemotherapy, seizure medications, and steroids, altering their levels in the body.
- Bleeding risk: A number of herbal and nutritional products can increase bleeding, which is critical to consider around brain surgery or if platelets are low.
- Immune and inflammation effects: Supplements that strongly stimulate or suppress immune function might interfere with immunotherapies or recovery from radiation.
- Dosing uncertainty: Over-the-counter products may vary in purity, potency, and quality control.
“In neuro-oncology, even small changes in bleeding risk, blood pressure, or sedation can have major consequences. We need to know exactly what patients are taking, including ‘natural’ supplements.”
— Neuro-oncology pharmacist
Practical Ways to Support Treatment While Research Continues
While the science on specific supplement combinations for glioblastoma is still evolving, there are evidence-informed steps patients and families can take right now to support overall care and quality of life.
1. Focus on what’s proven to matter
- Adhering closely to recommended surgery, radiation, and chemotherapy schedules.
- Managing symptoms like seizures, headaches, and mood changes promptly.
- Attending regular follow-up imaging and visits.
2. Consider supportive nutrition with professional guidance
A registered dietitian familiar with oncology can help tailor an eating plan that:
- Maintains strength and muscle mass.
- Respects swallowing difficulties or nausea.
- Coordinates safely with steroids and other medications.
3. Ask about clinical trials
If you’re interested in novel metabolic or supplement-based approaches, a clinical trial is the safest setting. Trials provide:
- Careful monitoring for side effects.
- Standardized doses and high-quality products.
- Oversight by ethics committees and regulatory bodies.

Real-World Obstacles: Hope, Hype, and Hard Decisions
Families facing glioblastoma often navigate a flood of online information—some carefully researched, some misleading, and some outright predatory. A few common challenges include:
- Overhyped headlines: News articles may imply that a lab finding translates directly into a treatment, which is rarely the case.
- Unregulated products: Supplements promoted as “miracle cures” are often expensive, poorly studied, and marketed with emotional testimonials rather than data.
- Decision fatigue: Caregivers can feel pressure to “try everything,” even when it adds stress and complexity without clear benefit.
One caregiver I worked with through a patient support group described keeping a spreadsheet of potential supplements, diets, and experimental approaches for her husband’s glioblastoma. After reviewing the list with their neuro-oncologist, they narrowed it to:
- Enrolling in a clinical trial that fit his tumor type.
- Adding only one basic, medically approved supplement to correct a documented deficiency.
- Focusing energy on physical therapy, family time, and symptom management instead of chasing every new headline.
She later shared that saying “no” to many unproven options was difficult, but it ultimately made their days more manageable and meaningful.
A “Before and After” Perspective: Headlines vs. Informed Action
It may help to think of your response to stories like the supplement-combo study in terms of a “before and after” mindset shift:
- Reading a headline and feeling either desperate hope or deep skepticism.
- Considering buying supplements immediately “just in case.”
- Feeling alone in trying to interpret complex science.
- Recognizing early research as a sign that smart people are working hard on this disease.
- Bringing new findings to your oncology team for context and safety checks.
- Using reliable sources and support networks to weigh benefits, risks, and trade-offs.
Moving Forward With Cautious Hope
The supplement-combination research featured by ScienceAlert adds to a growing body of work suggesting that glioblastoma’s unique metabolism can be exploited—and that some tools might already be on pharmacy shelves. That’s genuinely hopeful news.
At the same time, we are not yet at a point where any over-the-counter supplement combo can be recommended as a proven treatment for glioblastoma. The safest and most powerful steps you can take today are:
- Staying closely connected with a specialized neuro-oncology team.
- Discussing any supplement or diet idea with your clinicians before you act.
- Exploring clinical trial options that align with your values and goals.
- Leaning on supportive care—nutrition, rehab, mental health, and palliative care—early, not just in crisis.
If you’ve recently read about this supplement combo and are wondering what it means for you or someone you love, a practical next step is simple:
At your next appointment, bring the article (or a printout) and ask: “How does this apply to my situation, if at all?”
You deserve clear, compassionate, and evidence-informed guidance. Research is moving forward; your choices today can be grounded in both hope and safety.

